Part of the Ortho NI Group
At Hip NI, we perform hundreds of procedures every year with consistently high patient satisfaction. With a proven record of effective treatment and recovery management, you can be sure you are in the best of care at Hip NI.
You can be sure you are in the best of care with Ortho NI’s leading hip specialists.
The extensive experience of our award-winning consultants, Mr Dennis Molloy, Mr Pooler Archbold and Mr Roger Wilson covers a comprehensive range of orthopaedic procedures.

Hip Arthritis
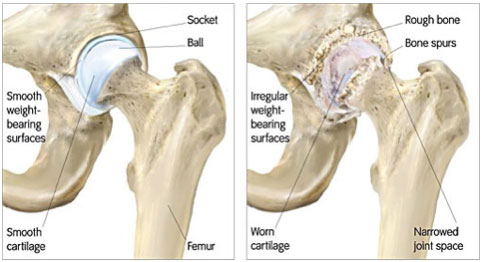
Also known as: Arthritis, Arthrosis, Wear & Tear, Hip arthritis is a general term covering numerous conditions where the joint surface (articular cartilage) of the hip wears out. When this occurs, the bone ends rub together and this is painful. In general it affects people as they age (Osteoarthritis-wear and tear arthritis). This can be associated with shortening of the effected limb.
Possible Causes
Although it is typically thought of as a ‘wear and tear’ phenomenon the exact cause of osteoarthritis is generally unknown. However several risk factors have been identified these include;
- Age: The risk of developing arthritis increases with age
- Genetic: specific genes are associated with a higher risk
- Overweight: Excess weight increases the load across the knee and contributes to the progression of arthritis. Weight loss can make a dramatic change to the level of your knee pain.
- Joint injuries – previous damage to the joint can contribute to the risk of developing arthritis
- Congenital abnormalities – hip dysplasia or shallow hips, previous injuries to the hips as a child can predispose you to the development of osteoarthritis.
Rheumatoid arthritis is a widespread disease found throughout the body in which the patients own immune system mistakenly attacks the joints causing widespread inflammation and damage.
Symptoms
The main symptoms of osteoarthritis of the hip are:
- Pain – increased on activity or at the end of the day, usually felt in the groin or anterior thigh.
- Stiffness, especially during the first few steps.
- Creaking, crunching, crepitus sensation when you move your hip

Diagnosis
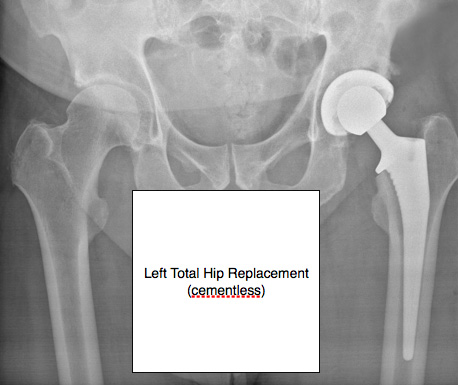
Osteoarthritis of the hip is diagnosed by a clinical examination and the history of your symptoms. X-rays are useful to evaluate the extent of any damage and help your doctor decide the most suitable treatment. The X rays will show a narrowing of the space between the bones in your hip (see below). This indicates the extent of wear to your articular cartilage. Joint replacement is usually only indicated if bone on bone is present on the X ray.
Treatment
As yet there’s no cure for osteoarthritis, but there are a number of treatments that can help ease symptoms and reduce the chances of your arthritis becoming worse.
Conservative Management
Non-operative treatment should always be exhausted prior to proceeding with any form of surgery. Possible non-operative options available include:
- Weight loss
- Physiotherapy- to prevent any further stiffness and regain range of motion
- Painkillers and anti-inflammatories – mild/ moderate pain killers and anti-inflammatory medications may be taken to provide symptomatic relief.
Surgery
The form of surgery chosen should be the least invasive approach required to provide long-term pain relief and restore function.
- Hip Replacement : Ultimately in cases of severe non-resolvable pain or previous failed treatment options, hip replacement (arthroplasty) is indicated. There are a number of hip replacements available. The choice of replacement depends on a number of criteria these include: the surgeon’s preference, age, activity level, form of arthritis, and the amount of bone affected.
Hip replacements are largely successful operations with good long-term outcomes.
Femero-acetabular impingement
Femoroacetabular impingement (FAI) is a condition where the bones of the hip are abnormally shaped. Because they do not fit together perfectly, the hip bones rub against each other and cause damage to the joint.
Types of FAI
There are three types of FAI: pincer, cam, and combined impingement.
Pincer. This type of impingement occurs because extra bone extends out over the normal rim of the acetabulum. The labrum can be crushed under the prominent rim of the acetabulum.
CAM. In CAM impingement the femoral head is not round and cannot rotate smoothly inside the acetabulum. A bump forms on the edge of the femoral head that grinds the cartilage inside the acetabulum.
Combined. Combined impingement just means that both the pincer and cam types are present
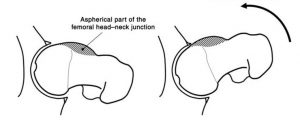
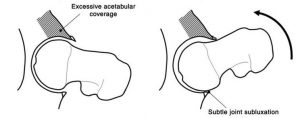
(left) FAI caused by presence of CAM lesion on femoral neck (right) caused by pincer lesion
Labral detachment/ tear can occur due to an acute injury or repeated impingement.

Treatment – femero-acetabular impingement
Nonsurgical Treatment
Activity changes. Your doctor may first recommend simply changing your daily routine and avoiding activities that cause symptoms.
Non-steroidal anti-inflammatory medications. Drugs like ibuprofen can be provided in a prescription-strength form to help reduce pain and inflammation.
Physical therapy. Specific exercises can improve the range of motion in your hip and strengthen the muscles that support the joint. This can relieve some stress on the injured labrum or cartilage.
Surgical Treatment
If tests show joint damage caused by FAI and your pain is not relieved by nonsurgical treatment, your doctor may recommend surgery.
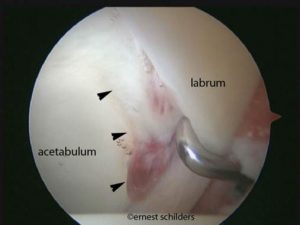
Many FAI problems can be treated with arthroscopic surgery. Arthroscopic procedures are done with small incisions and thin instruments. The surgeon uses a small camera, called an arthroscope, to view inside the hip.
During arthroscopy, your doctor can repair or clean out any damage to the labrum and articular cartilage. He can correct the FAI by trimming the bony rim of the acetabulum and also shaving down the bump on the femoral head. Some severe cases may require an open operation with a larger incision to accomplish this.
Trochanteric Bursitis
What is the trochanteric bursa?
In many areas of the body, muscles and tendons must slide over and against one another during movement. At each of these places, a small sac of lubricating fluid helps the muscles and tendons move properly. One of these places is the hip. Usually these sacs of fluid, called bursa function to reduce friction. The hip bone is one such area in the body.
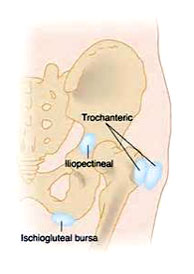
What is trochanteric (hip) bursitis?
Trochanteric bursitis is a common problem that causes pain in the area of the hip over the bump that forms the greater trochanter. Eventually the pain may radiate down the outside of the thigh. When the bursa sac becomes inflamed, pain results each time the tendon has to move over the bone. The pain may eventually be present at rest and may even cause a problem sleeping.
What causes trochanteric (hip) bursitis?
Most cases of trochanteric (hip) bursitis appear gradually with no obvious underlying injury or cause. Trochanteric (hip) bursitis may occur after hip surgery. A fall on the hip may also injure the bursa.
How is trochanteric (hip) bursitis diagnosed?
The diagnosis begins with a history and physical examination. In fact, this is usually all that is necessary to make the diagnosis.
Treatment of trochanteric bursitis.
Treatment usually consists of the following:
- Use of heat & ice – 1 min alternate for half an hour every evening
- Use of regular NSAIDs
- Pilates and core strengthening exercises – physiotherapy
- Steroid injection
Snapping Hip Syndrome
The occasional “snapping” that can be heard when walking or moving your leg results from the movement of a muscle or tendon (the tough, fibrous tissue that connects muscle to bone) over a bony structure. In the hip, the most common site is at the outer side where a band of connective tissue (the iliotibial band) passes over the broad, flat portion of the thighbone known as the greater trochanter. The snapping can also occur from the back-and-forth motion that takes place when the tendon, running from the inside of the thighbone (femur) up through the pelvis, shifts across the head of the femur. A tear in the cartilage or some bone debris in the hip joint can also cause a snapping or clicking sensation.
Investigation
A detailed history and examination can provide your physician with most of the information to make a diagnosis of snapping hip syndrome. This can be confirmed with specific investigations
An ultrasound of the effected area can show thickening of the overlying tissues in this condition. Magnetic Resonance Scanning (MRI) can confirm the diagnosis of snapping hip syndrome
Treatment
The vast majority of cases can be treated effectively by physiotherapy, involving stretching of the effected soft tissue, strengthening and alignment treatment. Sometimes, treatment with a corticosteroid injection to the area can relieve inflammation.
Avascular Necrosis of the Femoral Head
Avascular necrosis (AVN) (also known as osteonecrosis) is a condition in which the bone loses blood circulation to an area of bone. In extreme cases, it can result in the collapse of a segment of bone. When the surface of a joint is involved, it may lead to rapidly progressive osteoarthritis.
Avascular necrosis can occur as a result of an injury that interrupts the blood supply, such as in AVN of the hip after a fracture of the neck of femur (thighbone). Other causes include the use of systemic steroids as well as certain inflammatory diseases, such as lupus. The exact mechanism for loss of circulation in these circumstances is not well understood.
The most common body parts affected by AVN are the hip and knee. In cases of AVN of the hip, it is very important to diagnose and treat early in order to prevent disability. Treatment varies considerably, depending on the location and severity, but the goal of initial treatment is to prevent collapse of the joint surface. In the advanced stages that result in painful arthritis, a hip replacement may become necessary.
Listed are the most common procedures performed on the hip.
Total Hip Replacement
A hip replacement is a common type of surgery where a damaged hip joint is replaced with an artificial one (known as a prosthesis).
Adults of any age can be considered for a hip replacement, although most are carried out on people between the ages of 60 and 80.
A modern artificial hip joint is designed to last for at least 15 years. Most people experience a significant reduction in pain and some improvement in their range of movement.
Hip replacement surgery is usually necessary when the hip joint is worn or damaged to the extent that your mobility is reduced and you experience pain even while resting.
The most common reason for hip replacement surgery is osteoarthritis. Other conditions that can cause hip joint damage include:
- rheumatoid arthritis
- a hip fracture
- septic arthritis (infection)
- ankylosing spondylitis
- disorders that cause unusual bone growth (bone dysplasia).
A hip replacement is major surgery, so is normally only recommended if other treatments, such as physiotherapy or steroid injections, haven’t helped reduce pain or improve mobility.
You may be offered hip replacement surgery if:
- you have severe pain, swelling and stiffness in your hip joint and your mobility is reduced
- your hip pain is so severe that it interferes with your quality of life and sleep
- everyday tasks, such as shopping or getting out of the bath, are difficult or impossible
- you’re feeling depressed because of the pain and lack of mobility
- you can’t work or have a normal social life
You’ll also need to be well enough to cope with both a major operation and the rehabilitation afterwards.
Hip Replacement Surgery
A hip replacement can be carried out under a general anaesthetic (where you’re asleep during the procedure) or a spinal anaesthetic (where the lower body is numbed). We recommend a spinal anaesthetic as this is a safe procedure that give good post-operative pain relief.
The surgeon makes an incision into the hip, removes the damaged hip joint and replaces it with an artificial joint made of a metal alloy or, in some cases, ceramic.
The surgery usually takes around 50-70 minutes to complete.
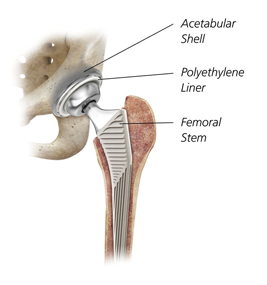
Cementless Total Hip replacement
Animation courtesy Visual Health Solutions, Inc.
Post-operative
The rehabilitation process after surgery can be a demanding time and requires commitment. You will mobilise with help the same day or the day after your operation. You will be given adequate analgesia to make this as comfortable as possible.
You will be given a daily injection for 4 weeks after your hip replacement, in keeping with national guidelines, to reduce the risk of developing a complication from Deep Venous Thrombosis formation.
For the first four to six weeks after the operation you may need a walking aid, such as crutches, to help support you.
You may also be enrolled on an exercise programme that’s designed to help you regain and then improve the use of your new hip joint.
Most people are able to resume normal activities within two to three months but it can take up to a year before you experience the full benefits of your new hip.
Complications of a hip replacement can include:
- hip dislocation
- infection at the site of the surgery
- injuries to the blood vessels or nerves
- a fracture
- differences in leg length
However, the risk of serious complications is low – estimated to be less than 1 in a 100.
Aseptic Loosening
The most common problem that can arise as a result of a hip replacement is loosening of the joint, which causes pain and feeling that the joint is unstable. This happens in around 10% of cases.
This can be caused by the shaft of the prosthesis becoming loose in the hollow of the thigh bone, or due to thinning of the bone around the implant.
Loosening of the joint can occur at any time, but it normally occurs 10-15 years after the original surgery was performed.
Another operation (revision surgery) may be necessary, although this can’t be performed in all patients.
Hip Dislocation
In around 1-3% of cases the hip joint can come out of its socket. This is most likely to occur in the first few months after surgery when the hip is still healing.
Further surgery will be required to put the joint back into place.
Wear and tear
Another common complication of hip replacement surgery is wear and tear of the artificial sockets. Particles that have worn off the artificial joint surfaces can be absorbed by surrounding tissue, causing loosening of the joint.
If wear or loosening is noticed on X-ray, your surgeon may request regular X-rays. Depending on the severity of the problem, you may be advised to have further surgery.
You can consult your doctor for further advice if you have any concerns about your hip replacement or don’t know which type you have.
Joint stiffening
The soft tissues can harden around the implant, causing reduced mobility.
This isn’t usually painful and can be prevented using medication or radiation therapy (a quick and painless procedure during which controlled doses of radiation are directed at your hip joint).
Serious complications
Serious complications of a hip replacement are uncommon, occurring in fewer than one in a 100 cases.
Blood clots
There’s a small risk of developing a blood clot in the first few weeks after surgery – either deep vein thrombosis (DVT) in the leg or pulmonary embolism in the lung.
Symptoms of DVT include:
- pain, swelling and tenderness in one of your legs (usually your calf)
- a heavy ache in the affected area
- warm skin in the area of the clot
Symptoms of pulmonary embolism include:
- breathlessness, which may come on suddenly or gradually
- chest pain, which may be worse when you breathe in
- coughing
If you suspect either of these types of blood clots you should seek immediate medical advice from your GP or the doctor in charge of your care. If this isn’t possible then call your local out-of-hours service.
To reduce your risk of blood clots you may be given blood thinning medication such as clexane, or asked to wear compression stockings.
Infection
There’s always a small risk that some bacteria could work its way into the tissue around the artificial hip joint, triggering an infection.
Symptoms of an infection include:
- a high temperature (fever) of 38C (100.4F) or above
- shaking and chills
- redness and swelling at the site of the surgery
- a discharge of liquid from the site of the surgery
- hip pain that can persist even when resting
Seek immediate medical advice, as detailed above, if you think you may have an infection
The National Joint Registry
The National Joint Registry (NJR) collects details of knee replacements carried out in England and Wales. Although it’s voluntary, it’s worth registering. This enables the NJR to monitor knee replacements, so you can be identified if any problems emerge in the future.
The registry also gives you the chance to participate in a patient feedback survey.
It’s confidential and you have a right under the Freedom of Information Act to see what details are kept about you.
Hip Arthroscopy
Arthroscopy is a surgical procedure that gives doctors a clear view of the inside of a joint. This helps them diagnose and treat hip problems.
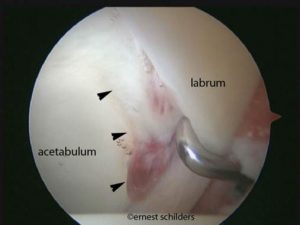
During hip arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your hip joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments. This can be used to treat a number of hip conditions.
Hip arthroscopy has been performed for many years, but is not as common as knee or shoulder arthroscopy.
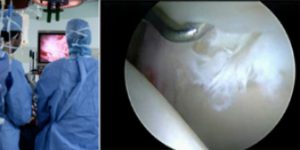
During arthroscopy, your surgeon can see the structures of your hip in great detail. (Right) Small instruments are used to repair a labral tear.
Anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A slippery tissue called articular cartilage covers the surface of the ball and the socket. It creates a smooth, frictionless surface that helps the bones glide easily across each other.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket. This is thought to help form a fluid seal.
The joint is surrounded by bands of tissue called ligaments. They form a capsule that holds the joint together.
The under surface of the capsule is lined by a thin membrane called the synovium. It produces synovial fluid that lubricates the hip joint.
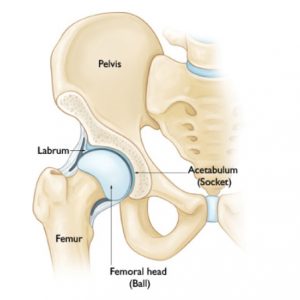
In a healthy hip, the femoral head fits perfectly into the acetabulum.
When Hip Arthroscopy Is Recommended
Your doctor may recommend hip arthroscopy if you have a painful condition that does not respond to nonsurgical treatment. Nonsurgical treatment includes rest, physical therapy, and medications or injections that can reduce inflammation. Inflammation is one of your body’s normal reactions to injury or disease. In an injured or diseased hip joint, inflammation causes swelling, pain, and stiffness.
Hip arthroscopy may relieve painful symptoms of many problems that damage the labrum, articular cartilage, or other soft tissues surrounding the joint. Although this damage can result from an injury, other orthopaedic conditions can lead to these problems, such as:
- Femoroacetabular impingement (FAI) is a disorder where bone spurs (bone overgrowth) around the socket or the femoral head cause damage.
- Labral tear
- Dysplasia is a condition where the socket is abnormally shallow and makes the labrum more susceptible to tearing.
- Snapping hip syndromes cause a tendon to rub across the outside of the joint. This type of snapping or popping is often harmless and does not need treatment. In some cases, however, the tendon is damaged from the repeated rubbing.
- Synovitis causes the tissues that surround the joint to become inflamed.
- Loose bodies are fragments of bone or cartilage that become loose and move around within the joint.
- Hip joint infection
Planning for Surgery
If you are having arthroscopy, you will need a physical examination from a physician to assess your health. He or she will identify any problems that may interfere with the surgery.
If you have certain health risks, a more extensive evaluation may be necessary before your surgery. Be sure to inform your orthopaedic surgeon of any medications or supplements that you take. He or she may tell you which medications to stop and which to take prior to surgery.
If you are generally healthy, your hip arthroscopy will most likely be performed as an outpatient. This means you will not need to stay overnight at the hospital.
The hospital or surgery centre will contact you ahead of time to provide specific details of your procedure. Make sure to follow the instructions on when to arrive and especially on when to stop eating or drinking prior to your procedure.
You will be asked to fill in a number of questionnaires which will be submitted to a national data base. You will be asked to participate in this registry post-operatively filling in the same questionnaires at certain times after your surgery (https://www.britishhipsociety.com/main?page=NAHR)
Before the operation, you will also be evaluated by a member of the anaesthesia team. Hip arthroscopy is most commonly performed under general anaesthesia, where you go to sleep for the operation. You will be asked to complete pre-operative questionnaires relating to your hip function and pain. You will be invited to participate in The Non-arthroplasty Hip Registry, a nation-wide registry evaluating the outcome of hip surgery.
Surgical Procedure
At the start of the procedure, your leg will be put in traction. This means that your hip will be pulled away from the socket enough for your surgeon to insert instruments, see the entire joint, and perform the treatments needed.
After traction is applied, your surgeon will make a small puncture in your hip (about the size of a buttonhole) for the arthroscope. Through the arthroscope, he or she can view the inside of your hip and identify damage.

(Left) Your surgeon inserts the arthroscope through a small incision about 1-1.5cm. (Right) Other instruments are inserted to treat the problem. You may have up to 3 incisions in total
Your surgeon will insert other instruments through separate incisions to treat the problem. A range of procedures can be done, depending on your needs. For example, your surgeon can:
- Smooth off torn cartilage or repair it
- Trim bone spurs caused by FAI
- Remove inflamed synovial tissue
The length of the procedure will depend on what your surgeon finds and the amount of work to be done. If adequate clearance of bone cannot be achieved through the keyhole technique a small incision (5-8cm) may be used to open the joint.
Complications
Complications from hip arthroscopy are uncommon. Any surgery in the hip joint carries a small risk of injury to the surrounding nerves or vessels, or the joint itself. The traction needed for the procedure can stretch nerves and cause numbness in the perineal region (groin), but this is usually temporary.
There are also small risks of infection, as well as blood clots forming in the legs (deep vein thrombosis).
Recovery
After surgery, you will stay in the recovery room for 1 to 2 hours before being discharged to the ward. You usually stay in hospital overnight although this is not mandatory. You can also expect to be on crutches, for some period of time depending on the procedure performed (usually 4 weeks).
Rehabilitation
Your surgeon will develop a rehabilitation plan based on the surgical procedures you required. In some cases, crutches are necessary, but only until any limping has stopped. If you required a more extensive procedure, however, you may need crutches for 1 to 2 months.
In most cases, physical therapy is necessary to achieve the best recovery. Specific exercises to restore your strength and mobility are important. Your therapist can also guide you with additional do’s and don’ts during your rehabilitation.
Long-Term Outcomes
Many people (70 – 80%) return to full, unrestricted activities after arthroscopy. Your recovery will depend on the type of damage that was present in your hip.
For some people, lifestyle changes are necessary to protect the joint. An example might be changing from high impact exercise (such as running) to lower impact activities (such as swimming or cycling). These are decisions you will make with the guidance of your surgeon.
Sometimes, the damage can be severe enough that it cannot be completely reversed and the procedure may not be successful.
Trochanteric Bursa Injection
How is this injection performed?
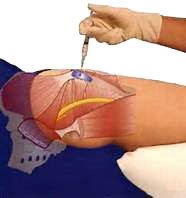 If your doctor uses ultrasound guidance, the nurse will position you on your side. Occasionally your doctor may perform the procedure without the use of ultrasound.
If your doctor uses ultrasound guidance, the nurse will position you on your side. Occasionally your doctor may perform the procedure without the use of ultrasound.
Your doctor will clean the area to be injected with an antibacterial solution. They will guide the needle to the greater trochanter. When they are satisfied with the needle placement, he will inject the medication into the area and remove the needle.
The nurse will clean the antibacterial solution off your skin and apply a dressing if needed.
-
Just a brief note to record my sincere appreciation for all your professional skills and personal attention. I look forward to getting out and about again very soon. Thanks for everything.
S.W.
-
Please accept my very grateful thanks for the professional and caring way you treated me during my recent hip replacement surgery. It was very reassuring to know that I was in a very 'safe pair of hands' and that I will soon be back to my normal, active self.
B.B.
-
Thank you so much for all your help. Your professional, approachable manner was second to none. With best wishes.
P.J.
-
Very many thanks for your wonderful care and attention given to me in my recent operation. It was really helpful to be kept informed of what was happening, and overall I found the experience an enjoyable one. Thanks and Best wishes.
D.H.
All of our practitioners are approved by leading insurance companies

Cookie Policy
This site uses cookies in the interest of providing the best user experience. If you continue without changing your settings, it will be assumed that you are happy to receive all cookies from the andyhenry.co.uk site. If you do not wish to receive cookies from this site, you are free to change your cookie settings at any time.