Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel.
The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump.
Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration.
Description
Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body’s natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed.
Noninsertional Achilles tendinitis
Noninsertional Achilles Tendinitis
In noninsertional Achilles tendinitis, fibers in the middle portion of the tendon have begun to break down with tiny tears (degenerate), swell, and thicken.
Tendinitis of the middle portion of the tendon more commonly affects younger, active people.
Insertional Achilles Tendinitis
Insertional Achilles tendinitis involves the lower portion of the heel, where the tendon attaches (inserts) to the heel bone.
In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Bone spurs (extra bone growth) often form with insertional Achilles tendinitis.
Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Insertional Achilles tendinitis
Cause
Achilles tendinitis is typically not related to a specific injury. The problem results from repetitive stress to the tendon. This often happens when we push our bodies to do too much, too soon, but other factors can make it more likely to develop tendinitis, including:
A bone spur that has developed where the tendon attaches to the heel bone.
- Sudden increase in the amount or intensity of exercise activity—for example, increasing the distance you run every day by a few miles without giving your body a chance to adjust to the new distance
- Tight calf muscles—Having tight calf muscles and suddenly starting an aggressive exercise program can put extra stress on the Achilles tendon
- Bone spur—Extra bone growth where the Achilles tendon attaches to the heel bone can rub against the tendon and cause pain
Symptoms
Common symptoms of Achilles tendinitis include:
- Pain and stiffness along the Achilles tendon in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Severe pain the day after exercising
- Thickening of the tendon
- Bone spur (insertional tendinitis)
- Swelling that is present all the time and gets worse throughout the day with activity
If you have experienced a sudden “pop” in the back of your calf or heel, you may have ruptured (torn) your Achilles tendon. See your doctor immediately if you think you may have torn your tendon.
Examination
After you describe your symptoms and discuss your concerns, the doctor will examine your foot and ankle. The doctor will look for these signs:
- Swelling along the Achilles tendon or at the back of your heel
- Thickening or enlargement of the Achilles tendon
- Bony spurs at the lower part of the tendon at the back of your heel (insertional tendinitis)
- The point of maximum tenderness
- Pain in the middle of the tendon, (noninsertional tendinitis)
- Pain at the back of your heel at the lower part of the tendon (insertional tendinitis)
- Limited range of motion in your ankle—specifically, a decreased ability to flex your foot
Tests
Your doctor may order imaging tests to make sure your symptoms are caused by Achilles tendinitis.
X-rays
X-ray tests provide clear images of bones. X-rays can show whether the lower part of the Achilles tendon has calcified, or become hardened. This calcification indicates insertional Achilles tendinitis. In cases of severe noninsertional Achilles tendinitis, there can be calcification in the middle portion of the tendon, as well.
Magnetic Resonance Imaging (MRI)
Although magnetic resonance imaging (MRI) is not necessary to diagnose Achilles tendinitis, it is important for planning surgery. An MRI scan can show how severe the damage is in the tendon. If surgery is needed, your doctor will select the procedure based on the amount of tendon damage.
Treatment
Nonsurgical Treatment
In most cases, nonsurgical treatment options will provide pain relief, although it may take a few months for symptoms to completely subside. Even with early treatment, the pain may last longer than 3 months. If you have had pain for several months before seeking treatment, it may take 6 months before treatment methods take effect.
Rest. The first step in reducing pain is to decrease or even stop the activities that make the pain worse. If you regularly do high-impact exercises (such as running), switching to low-impact activities will put less stress on the Achilles tendon. Cross-training activities such as biking, elliptical exercise, and swimming are low-impact options to help you stay active.
Ice. Placing ice on the most painful area of the Achilles tendon is helpful and can be done as needed throughout the day. This can be done for up to 20 minutes and should be stopped earlier if the skin becomes numb. A foam cup filled with water and then frozen creates a simple, reusable ice pack. After the water has frozen in the cup, tear off the rim of the cup. Then rub the ice on the Achilles tendon. With repeated use, a groove that fits the Achilles tendon will appear, creating a “custom-fit” ice pack.
Non-steroidal anti-inflammatory medication. Drugs such as ibuprofen and naproxen reduce pain and swelling. They do not, however, reduce the thickening of the degenerated tendon. Using the medication for more than 1 month should be reviewed with your primary care doctor.
Exercise. The following exercise can help to strengthen the calf muscles and reduce stress on the Achilles tendon.
- Calf stretch
Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch.
Physical Therapy. Physical therapy is very helpful in treating Achilles tendinitis. It has proven to work better for noninsertional tendinitis than for insertional tendinitis.
Eccentric Strengthening Protocol. Eccentric strengthening is defined as contracting (tightening) a muscle while it is getting longer. Eccentric strengthening exercises can cause damage to the Achilles tendon if they are not done correctly. At first, they should be performed under the supervision of a physical therapist. Once mastered with a therapist, the exercises can then be done at home. These exercises may cause some discomfort, however, it should not be unbearable.
-
- Bilateral heel drop
Stand at the edge of a stair, or a raised platform that is stable, with just the front half of your foot on the stair. This position will allow your heel to move up and down without hitting the stair. Care must be taken to ensure that you are balanced correctly to prevent falling and injury. Be sure to hold onto a railing to help you balance.
Lift your heels off the ground then slowly lower your heels to the lowest point possible. Repeat this step 20 times. This exercise should be done in a slow, controlled fashion. Rapid movement can create the risk of damage to the tendon. As the pain improves, you can increase the difficulty level of the exercise by holding a small weight in each hand.
- Single leg heel drop
This exercise is performed similarly to the bilateral heel drop, except that all your weight is focused on one leg. This should be done only after the bilateral heel drop has been mastered.
Cortisone injections. Cortisone, a type of steroid, is a powerful anti-inflammatory medication. Cortisone injections into the Achilles tendon are rarely recommended because they can cause the tendon to rupture (tear).
Supportive shoes and orthotics. Pain from insertional Achilles tendinitis is often helped by certain shoes, as well as orthotic devices. For example, shoes that are softer at the back of the heel can reduce irritation of the tendon. In addition, heel lifts can take some strain off the tendon.
Heel lifts are also very helpful for patients with insertional tendinitis because they can move the heel away from the back of the shoe, where rubbing can occur. They also take some strain off the tendon. Like a heel lift, a silicone Achilles sleeve can reduce irritation from the back of a shoe.
If your pain is severe, your doctor may recommend a walking boot for a short time. This gives the tendon a chance to rest before any therapy is begun. Extended use of a boot is discouraged, though, because it can weaken your calf muscle.
Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged tendon tissue. ESWT has not shown consistent results and, therefore, is not commonly performed.
ESWT is noninvasive—it does not require a surgical incision. Because of the minimal risk involved, ESWT is sometimes tried before surgery is considered.
Surgical Treatment
Surgery should be considered to relieve Achilles tendinitis only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of the tendinitis and the amount of damage to the tendon.
Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, despite consistent stretching.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope—an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs.
Complication rates for gastrocnemius recession are low, but can include nerve damage.
Gastrocnemius recession can be performed with or without débridement, which is removal of damaged tissue.
Débridement and repair (tendon has less than 50% damage). The goal of this operation is to remove the damaged part of the Achilles tendon. Once the unhealthy portion of the tendon has been removed, the remaining tendon is repaired with sutures, or stitches to complete the repair.
In insertional tendinitis, the bone spur is also removed. Repair of the tendon in these instances may require the use of metal or plastic anchors to help hold the Achilles tendon to the heel bone, where it attaches.
After débridement and repair, most patients are allowed to walk in a removable boot or cast within 2 weeks, although this period depends upon the amount of damage to the tendon.
Débridement with tendon transfer (tendon has greater than 50% damage). In cases where more than 50% of the Achilles tendon is not healthy and requires removal, the remaining portion of the tendon is not strong enough to function alone. To prevent the remaining tendon from rupturing with activity, an Achilles tendon transfer is performed. The tendon that helps the big toe point down is moved to the heel bone to add strength to the damaged tendon. Although this sounds severe, the big toe will still be able to move, and most patients will not notice a change in the way they walk or run.
Depending on the extent of damage to the tendon, some patients may not be able to return to competitive sports or running.
Recovery. Most patients have good results from surgery. The main factor in surgical recovery is the amount of damage to the tendon. The greater the amount of tendon involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity.
Physical therapy is an important part of recovery. Many patients require 12 months of rehabilitation before they are pain-free.
Complications. Moderate to severe pain after surgery is noted in 20% to 30% of patients and is the most common complication. In addition, a wound infection can occur and the infection is very difficult to treat in this location.
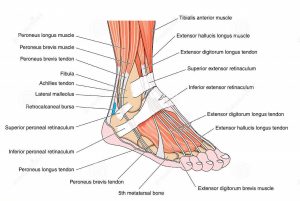
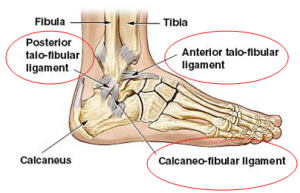
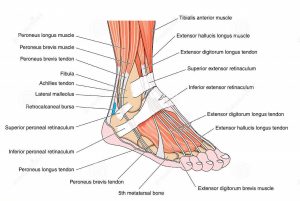
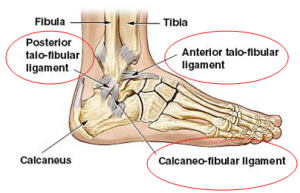
The ankle joint is a hinge between the leg and the foot. The bones of the leg (tibia and fibula) form a sort of slot and the curved top bone of the foot (talus) fits between them. The talus is held to the tibia and fibula by strong bands of tissue called ligaments. Each ligament is made of many strands or fibres of a material called collagen, which is extremely strong.
The ligament on the inside of the ankle (medial or deltoid ligament) has two layers; the deepest one is most important. This ligament is mainly torn in association with severe fractures of the ankle bones.
The ligament on the outside of the ankle (lateral ligament) is made up of three separate bands: one at the front (anterior talo-fibular ligament), one in the middle (calcaneo-fibular ligament) and one at the back (posterior talo-fibular ligament). The front band is the usual ligament injured in sprains or tears of the ankle ligaments, and the middle band is sometimes affected.
The tibia and fibula have a small joint between themselves just above the ankle. This also has strong ligaments, one at the front and one at the back. (tibio-fibular ligaments). The ligament at the front is involved in 10-20% of ankle sprains; the ligament at the back, like the deltoid ligament, is mainly damaged in association with severe fractures of the ankle bones.
How do they get injured?
Most ankle ligament injuries are caused when the foot twists so that the sole is pointing inwards (inversion), usually when the foot is pointing downwards rather than flat on the ground. When this happens, the full force of the body’s movement is placed on the anterior talo-fibular ligament. This may stretch, with tearing of some of its fibres (sprain) or it may tear completely. If there is a major injury of the anterior talo-fibular ligament, the forces transfer to the calcaneo-fibular ligament and the tibio-fibular ligaments, which may also be sprained or torn. Occasionally small pieces of bone may be torn off with the ligaments.
In a few cases, a twisting force on the ankle may cause other damage. The bones around the ankle may be broken, a piece of the joint surface inside the ankle may be chipped off, ligaments connecting other bones in the foot may be sprained or torn, or the tendons around the ankle may be damaged.
What should I do if I sprain my ankle?
Most ankle sprains are fairly minor injuries which will get better with simple self-care treatment. The word RICE reminds us of the basic treatment of a sprained joint:
- Rest take the weight off the injured joint as much as possible for a day or two
- Ice an ice pack (a small bag of frozen peas or corn is ideal) can be applied for 10-15 minutes 3-4 times a day to reduce swelling
- Compression a firm bandage or strapping will help to get swelling down
- Elevation resting with the ankle above the height of the body will allow swelling to drain away into the bloodstream
Although a couple of days rest is useful, it is best to start taking some weight on the injured ankle reasonably soon after injury, usually within 2-3 days. Also start to exercise and stretch the injured ankle as soon as possible after the injury.
Normally a sprained ankle will recover within 6-8 weeks, although it may tend to swell for a few weeks longer.
When should I go to casualty?
Basically, if you have a severe ankle injury it is best to get professional advice immediately. Things that suggest a severe injury include:
- your ankle is so painful you cannot bear any weight on it
- the ankle seems deformed
- the skin over the ankle is broken
- the injury was caused by a severe force such as a fall from a height or a blow from a heavy object
- the pain and swelling seem to get worse rather than better over the first 3-4 days (the bruising often gets worse for a week or more before it starts to fade)
Should I have physiotherapy?
Most simple sprains get better without any special treatment. However, if you have a severe injury or the initial injury does not recover normally, it is usually best to see a physiotherapist. The hospital casualty or orthopaedic department, your own GP or your sports club can arrange this. Physiotherapists also advertise in Yellow Pages and local papers.
Length of Recovery
Most ankle injuries get better completely and cause no long-term problems. Sometimes, however, there is some permanent damage to the ankle. The ligaments may fail to heal properly and become weak, or there may be damage to the joint itself or some other structure nearby.
Most importantly, an ankle ligament injury also damages the small nerve endings in the joint and ligaments. These endings are very important, as they tell your brain where your ankle is and what position it is in (they are called “proprioceptive nerves”). Your brain relies on this information to control the muscles which move and protect your ankle. If these nerve endings are not working properly, your brain does not get reliable information and the muscles around your ankle may not work together properly. You would feel this as a tendency for your ankle to “give way”, often with minor stresses. This might make you prone to repeated ankle sprains. This is referred to as “ankle instability” and is more commonly due to damage to the proprioceptive nerves than actual weakness of the ligaments.
How would ankle instability be diagnosed?
Your doctor or physiotherapist will listen to your complaints about your ankle and examine you. They will try to see if there is anything, which makes you more liable to ankle instability than average. They will look for any sign that you have some other problem around your ankle, such as damage to the joint surface. They will stretch your ankle in various directions to see if the ligaments are abnormally weak.
An Xray will usually be taken to see if there is any damage to the bones of your ankle. Ligaments do not show on Xrays. Ligament damage can be shown by taking Xrays with your ankle stretched in various directions (“stress views”), by injecting dye into your ankle or around a neighbouring tendon, or with a magnetic (MRI) scan. However, these special tests are usually not needed at first.
What can be done about ankle instability?
As most people with ankle instability have proprioceptive nerves which are not working properly, the first treatment is a physiotherapy programme to re-train these nerves how to respond to movements of the ankle, by doing various exercises and activities. If your ankle or Achilles tendon are stiff, you will also be shown exercises to stretch these, and the strength of the muscles around the ankle will be increased by exercises. If your foot shape makes you prone to extra stress on the ankle ligaments, a moulded insole may be advised for your shoe to reduce these stresses.
Many people will find their ankle much more stable and comfortable after physiotherapy. However, in some people problems continue. At this point the opinion of an orthopaedic foot and ankle surgeon would be helpful. If you have not already had the special tests mentioned above, these may be done now. The surgeon may also suggest an exploratory operation on your ankle (arthroscopy) to check on the state of the joint. If these tests suggest weakness of the ankle ligaments, an operation may be advised.
Will I need an operation?
Most people with ankle instability will not need an operation. Even if your ankle still feels unstable after physiotherapy, you could try a brace rather than having an operation to tighten up or replace the ligaments.
However, if no other treatment makes your ankle comfortable and tests show that the ligaments are weak, an operation may help. There are two main types of operation:
- the damaged ligaments are tightened up and re-attached to the bone – often known as the Brostrum procedure. This is suitable when the instability is not too severe. Its main advantage is that it causes less stiffness than the other type of repair, as it aims to achieve an anatomical repair of the ligaments.
- another piece of tissue, usually part of one of the nearby tendons, is borrowed and stitched between the bones where the ligaments should be. This is suitable when the instability is severe or you may put severe stresses on the repair. It is very strong but often causes quite a lot of stiffness in the ankle afterwards.
You would usually be in a plaster or brace for several weeks after an operation and would need further physiotherapy to help regain normal function.
The other problems which may occur after a ligament reconstruction operation include:
- pain in the ankle, either because of damage at the time of the original injury or because the ankle is now tighter than before
- numbness or tingling down the side of the foot due to stretching of one of the nerves either at the time of the original injury or the operation
- persistent swelling of the ankle
A bunion is a painful bony bump that develops on the inside of the foot at the big toe joint. Bunions are often referred to as hallux valgus.
Bunions develop slowly. Pressure on the big toe joint causes the big toe to lean toward the second toe. Over time, the normal structure of the bone changes, resulting in the bunion bump. This deformity will gradually increase and may make it painful to wear shoes or walk.
Anyone can get a bunion, but they are more common in women. Many women wear tight, narrow shoes that squeeze the toes together—which makes it more likely for a bunion to develop, worsen and cause painful symptoms.
In most cases, bunion pain is relieved by wearing wider shoes with adequate toe room and using other simple treatments to reduce pressure on the big toe.
Bunions sometimes develop in both feet.
The big toe is made up of two joints. The largest of the two is the metatarsophalangeal joint (MTP), where the first long bone of the foot (metatarsal) meets the first bone of the toe (phalanx).
Bunions develop at the MTP joint.
The metatarsophalangeal (MTP) joint.
Description
A bunion forms when the bones that make up the MTP joint move out of alignment: the long metatarsal bone shifts toward the inside of the foot, and the phalanx bones of the big toe angle toward the second toe. The MTP joint gets larger and protrudes from the inside of the forefoot.
The MTP joint becomes enlarged and inflamed.
The enlarged joint is often inflamed. The word “bunion” comes from the Greek word for turnip, and the bump on the inside of the foot typically looks red and swollen like a turnip.
Bunion Progression
Bunions worsen over time. As the big toe angles toward the second toe, it can cross over it and cause additional problems.
Bunions start out small — but they usually get worse over time (especially if the individual continues to wear tight, narrow shoes). Because the MTP joint flexes with every step, the bigger the bunion gets, the more painful and difficult walking can become.
An advanced bunion can greatly alter the appearance of the foot. In severe bunions, the big toe may angle all the way under or over the second toe. Pressure from the big toe may force the second toe out of alignment, causing it to come in contact with the third toe. Calluses may develop where the toes rub against each other, causing additional discomfort and difficulty walking.
Foot Problems Related to Bunions
In some cases, an enlarged MTP joint may lead to bursitis, a painful condition in which the fluid-filled sac (bursa) that cushions the bone near the joint becomes inflamed. It may also lead to chronic pain and arthritis if the smooth articular cartilage that covers the joint becomes damaged from the joint not gliding smoothly.
Adolescent Bunion
In addition to the common bunion, there are other types of bunions. As the name implies, bunions that occur in young people are called adolescent bunions. These bunions are most common in girls between the ages of 10 and 15.
While a bunion on an adult often restricts motion in the MTP joint, a young person with a bunion can normally move the big toe up and down. An adolescent bunion may still be painful, however, and make it difficult to wear shoes.
As opposed to adult bunions — which usually are associated with long-term wear of narrow, tight shoes — adolescent bunions are often genetic and run in families.
Bunionette
A bunionette, or “tailor’s bunion,” occurs on the outside of the foot near the base of the little toe. Although it is in a different spot on the foot, a bunionette is very much like a bunion. You may develop painful bursitis and a hard corn or callus over the bump.
A bunion that forms in the main joint of the little toe is called a bunionette.
Cause
Bunions may be caused by:
- Wearing poorly fitting shoes—in particular, shoes with a narrow, pointed toe box that forces the toes into an unnatural position
- Heredity—some people inherit feet that are more likely to develop bunions due to their shape and structure
- Having an inflammatory condition, such as rheumatoid arthritis, or a neuromuscular condition, such as polio
Symptoms
In addition to the visible bump on the inside of the foot, symptoms of a bunion may include:
- Pain and tenderness
- Redness and inflammation
- Hardened skin on the bottom of the foot
- A callus or corn on the bump
- Stiffness and restricted motion in the big toe, which may lead to difficulty in walking
Examination
Physical Examination
Your doctor will ask you about your medical history, general health, and symptoms. He or she will perform a careful examination of your foot. Although your doctor will probably be able to diagnose your bunion based on your symptoms and on the appearance of your toe, he or she will also order an x-ray.
X-Rays
X-rays provide images of dense structures, such as bone. An x-ray will allow your doctor to check the alignment of your toes and look for damage to the MTP joint.
The alignment of your foot bones changes when you stand or sit. Your doctor will take an x-ray while you are standing in order to more clearly see the malalignment of the bones of your foot. He or she will use the x-rays to determine how severe the bunion is, and how best to correct it.
X-rays of your foot will show your doctor how far out of alignment the bones have become.
Nonsurgical Treatment
In most cases, bunions are treated without surgery. Although nonsurgical treatment cannot actually “reverse” a bunion, it can help reduce pain and keep the bunion from worsening.
Changes in Footwear
In the vast majority of cases, bunion pain can be managed successfully by switching to shoes that fit properly and do not compress the toes. Some shoes can be modified by using a stretcher to stretch out the areas that put pressure on your toes. Your doctor can give you information about proper shoe fit and the type of shoes that would be best for you. (See below section on “Tips for Proper Shoe Fit”)
Padding
Protective “bunion-shield” pads can help cushion the painful area over the bunion. Pads can be purchased at a drugstore or pharmacy. Be sure to test the pads for a short time period first; the size of the pad may increase the pressure on the bump. This could worsen your pain rather than reduce it.
Orthotics and Other Devices
To take pressure off your bunion, your doctor may recommend that you wear over-the-counter or custom-made shoe inserts (orthotics). Toe spacers can be placed between your toes. In some cases, a splint worn at night that places your big toe in a straighter position may help relieve pain.
Icing
Applying ice several times a day for 20 minutes at a time can help reduce swelling. Do not apply ice directly on your skin.
Medications
Nonsteroidal anti-inflammatory medications such as ibuprofen and naproxen can help relieve pain and reduce swelling. Other medications can be prescribed to help pain and swelling in patients whose bunions are caused by arthritis.
When Is Bunion Surgery Needed?
Your doctor may recommend surgery for a bunion or bunionette if, after a period of time, you have pain and difficulty walking despite changes in footwear and other nonsurgical treatments. Bunion surgery realigns bone, ligaments, tendons, and nerves so that the big toe can be brought back to its correct position.
There are several surgical procedures to correct bunions. Although many are done on a same-day basis with no hospital stay, a long recovery is common after bunion surgery.
Surgery to remove an adolescent bunion is not recommended unless the bunion causes extreme pain that does not improve with a change in footwear or addition of orthotics. If an adolescent has bunion surgery, particularly before reaching skeletal maturity, there is a strong chance the bunion will return.
People often blame the common foot deformity claw toe on wearing shoes that squeeze your toes, such as shoes that are too short or high heels. However, claw toe also is often the result of nerve damage caused by diseases like diabetes or alcoholism, which can weaken the muscles in your foot. Having claw toe means your toes “claw,” digging down into the soles of your shoes and creating painful calluses. Claw toe gets worse without treatment and may become a permanent deformity over time.
- Your toes are bent upward (extension) from the joints at the ball of the foot.
- Your toes are bent downward (flexion) at the middle joints toward the sole of your shoe.
- Sometimes your toes also bend downward at the top joints, curling under the foot.
- Corns may develop over the top of the toe or under the ball of the foot.
Evaluation
If you have symptoms of a claw toe, see your doctor for evaluation. You may need certain tests to rule out neurological disorders that can weaken your foot muscles, creating imbalances that bend your toes. Trauma and inflammation can also cause claw toe deformity.
Treatment
Claw toe deformities are usually flexible at first, but they harden into place over time. If you have claw toe in early stages, your doctor may recommend a splint or tape to hold your toes in correct position. Additional advice:
- Wear shoes with soft, roomy toe boxes and avoid tight shoes and high-heels.
- Use your hands to stretch your toes and toe joints toward their normal positions.
- Exercise your toes by using them to pick up marbles or crumple a towel laid flat on the floor.
If you have claw toe in later stages and your toes are fixed in position:
- A special pad can redistribute your weight and relieve pressure on the ball of your foot.
- Try special “in depth” shoes that have an extra 3/8″ depth in the toe box.
- Ask a shoe repair shop to stretch a small pocket in the toe box to accommodate the deformity.
If these treatments do not help, you may need surgery to correct the problem.
Hammer Toe
A hammer toe is a deformity of the second, third or fourth toes. In this condition, the toe is bent at the middle joint, so that it resembles a hammer. Initially, hammer toes are flexible and can be corrected with simple measures but, if left untreated, they can become fixed and require surgery.
People with hammer toe may have corns or calluses on the top of the middle joint of the toe or on the tip of the toe. They may also feel pain in their toes or feet and have difficulty finding comfortable shoes.
Hammer toe results from shoes that don’t fit properly or a muscle imbalance, usually in combination with one or more other factors. Muscles work in pairs to straighten and bend the toes. If the toe is bent and held in one position long enough, the muscles tighten and cannot stretch out.
Shoes that narrow toward the toe may make your forefoot look smaller. But they also push the smaller toes into a flexed (bent) position. The toes rub against the shoe, leading to the formation of corns and calluses, which further aggravate the condition. A higher heel forces the foot down and squishes the toes against the shoe, increasing the pressure and the bend in the toe. Eventually, the toe muscles become unable to straighten the toe, even when there is no confining shoe.
Treatment
Conservative treatment starts with new shoes that have soft, roomy toe boxes. Shoes should be one-half inch longer than your longest toe. (Note: For many people, the second toe is longer than the big toe.) Avoid wearing tight, narrow, high-heeled shoes. You may also be able to find a shoe with a deep toe box that accommodates the hammer toe. Or, a shoe repair shop may be able to stretch the toe box so that it bulges out around the toe. Sandals may help, as long as they do not pinch or rub other areas of the foot.
Your doctor may also prescribe some toe exercises that you can do at home to stretch and strengthen the muscles. For example, you can gently stretch the toes manually. You can use your toes to pick things up off the floor. While you watch television or read, you can put a towel flat under your feet and use your toes to crumple it.
Finally, your doctor may recommend that you use commercially available straps, cushions or nonmedicated corn pads to relieve symptoms. If you have diabetes, poor circulation or a lack of feeling in your feet, talk to your doctor before attempting any self-treatment.
Hammer toe can be corrected by surgery if conservative measures fail. Usually, surgery is done on an outpatient basis with a local anesthetic. The actual procedure will depend on the type and extent of the deformity. After the surgery, there may be some stiffness, swelling and redness and the toe may be slightly longer or shorter than before. You will be able to walk, but should not plan any long hikes while the toe heals, and should keep your foot elevated as much as possible.
Heel Pain
Every mile you walk puts 60 tons of stress on each foot. Your feet can handle a heavy load, but too much stress pushes them over their limits. When you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues, you may develop heel pain, the most common problem affecting the foot and ankle. A sore heel will usually get better on its own without surgery if you give it enough rest. However, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it. When you continue to use a sore heel, it will only get worse and could become a chronic condition leading to more problems. Surgery is rarely necessary.
Heel pain can have many causes. If your heel hurts, see your doctor right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you’ve had it. Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel.
Treatment
Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Pain Beneath the Heel
If it hurts under your heel, you may have one or more conditions that inflame the tissues on the bottom of your foot:
- Stone bruise. When you step on a hard object such as a rock or stone, you can bruise the fat pad on the underside of your heel. It may or may not look discolored. The pain goes away gradually with rest.
- Plantar fasciitis (subcalcaneal pain). Doing too much running or jumping can inflame the tissue band (fascia) connecting the heel bone to the base of the toes. The pain is centered under your heel and may be mild at first but flares up when you take your first steps after resting overnight. You may need to do special exercises, take medication to reduce swelling and wear a heel pad in your shoe.
- Heel spur.When plantar fasciitis continues for a long time, a heel spur (calcium deposit) may form where the fascia tissue band connects to your heel bone. Your doctor may take an X-ray to see the bony protrusion, which can vary in size. Treatment is usually the same as for plantar fasciitis: rest until the pain subsides, do special stretching exercises and wear heel pad shoe inserts.
Pain Behind the Heel
If you have pain behind your heel, you may have inflamed the area where the Achilles tendon inserts into the heel bone (retrocalcaneal bursitis). People often get this by running too much or wearing shoes that rub or cut into the back of the heel. Pain behind the heel may build slowly over time, causing the skin to thicken, get red and swell. You might develop a bump on the back of your heel that feels tender and warm to the touch. The pain flares up when you first start an activity after resting. It often hurts too much to wear normal shoes. You may need an X-ray to see if you also have a bone spur.
Treatment includes resting from the activities that caused the problem, doing certain stretching exercises, using pain medication and wearing open back shoes.
- Your doctor may want you to use a 3/8″ or 1/2″ heel insert.
- Stretch your Achilles tendon by leaning forward against a wall with your foot flat on the floor and heel elevated with the insert.
- Use nonsteroidal anti-inflammatory medications for pain and swelling.
- Consider placing ice on the back of the heel to reduce inflammation.
Ingrown Toenail
If you trim your toenails too short, particularly on the sides of your big toes, you may set the stage for an ingrown toenail. Like many people, when you trim your toenails, you may taper the corners so that the nail curves with the shape of your toe. But this technique may encourage your toenail to grow into the skin of your toe. The sides of the nail curl down and dig into your skin. An ingrown toenail may also happen if you wear shoes that are too tight or too short.
When you first have an ingrown toenail, it may be hard, swollen and tender. Later, it may get red and infected, and feel very sore. Ingrown toenails are a common, painful condition—particularly among teenagers. Any of your toenails can become ingrown, but the problem more often affects the big toe. An ingrown nail occurs when the skin on one or both sides of a nail grows over the edges of the nail, or when the nail itself grows into the skin. Redness, pain and swelling at the corner of the nail may result and infection may soon follow. Sometimes a small amount of pus can be seen draining from the area.
Ingrown nails may develop for many reasons. Some cases are congenital—the nail is just too large for the toe. Trauma, such as stubbing the toe or having the toe stepped on, may also cause an ingrown nail. However, the most common cause is tight shoe wear or improper grooming and trimming of the nail.
The anatomy of a toenail.
Treatment
Nonsurgical Treatment
Ingrown toenails should be treated as soon as they are recognized. If they are recognized early (before infection sets in), home care may prevent the need for further treatment:
- Soak the foot in warm water 3-4 times daily.
- Keep the foot dry during the rest of the day.
- Wear comfortable shoes with adequate room for the toes. Consider wearing sandals until the condition clears up.
- You may take ibuprofen or acetaminophen for pain relief.
- If there is no improvement in 2-3 days, or if the condition worsens, call your doctor.
You may need to gently lift the edge of the ingrown toenail from its embedded position and insert some cotton or waxed dental floss between the nail and your skin. Change this packing every day.
Surgical Treatment
If excessive inflammation, swelling, pain and discharge are present, the toenail is probably infected and should be treated by a physician (see left image below). You may need to take oral antibiotics and the nail may need to be partially or completely removed (see middle image below). The doctor can surgically remove a portion of the nail, a portion of the underlying nail bed, some of the adjacent soft tissues and even a part of the growth center (see right image below).
Surgery is effective in eliminating the nail edge from growing inward and cutting into the fleshy folds as the toenail grows forward. Permanent removal of the nail may be advised for children with chronic, recurrent infected ingrown toenails.
If you are in a lot of pain and/or the infection keeps coming back, your doctor may remove part of your ingrown toenail (partial nail avulsion). Your toe is injected with an anesthetic and your doctor uses scissors to cut away the ingrown part of the toenail, taking care not to disturb the nail bed. An exposed nail bed may be very painful. Removing your whole ingrown toenail (complete nail plate avulsion) increases the likelihood your toenail will come back deformed. It may take 3-4 months for your nail to regrow.
Risk Factors
Unless the problem is congenital, the best way to prevent ingrown toenails is to protect the feet from trauma and to wear shoes and hosiery (socks) with adequate room for the toes. Nails should be cut straight across with a clean, sharp nail trimmer without tapering or rounding the corners. Trim the nails no shorter than the edge of the toe. Keep the feet clean and dry at all times.
Proper and improper toenail trimming.
Plantar Fasciitis and Bone Spurs
Plantar fasciitis is the most common cause of pain on the bottom of the heel. Plantar fasciitis occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed.
The plantar fascia is a long, thin ligament that lies directly beneath the skin on the bottom of your foot. It connects the heel to the front of your foot, and supports the arch of your foot.
Cause
The plantar fascia is designed to absorb the high stresses and strains we place on our feet. But, sometimes, too much pressure damages or tears the tissues. The body’s natural response to injury is inflammation, which results in the heel pain and stiffness of plantar fasciitis.
Risk Factors
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that can make you more prone to the condition:
- Tighter calf muscles that make it difficult to flex your foot and bring your toes up toward your shin
- Obesity
- Very high arch
- Repetitive impact activity (running/sports)
- New or increased activity
Heel Spurs
Although many people with plantar fasciitis have heel spurs, spurs are not the cause of plantar fasciitis pain. One out of 10 people has heel spurs, but only 1 out of 20 people (5%) with heel spurs has foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.
Heel spurs do not cause plantar fasciitis pain.
Symptoms
The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot near the heel
- Pain with the first few steps after getting out of bed in the morning, or after a long period of rest, such as after a long car ride. The pain subsides after a few minutes of walking
- Greater pain after (not during) exercise or activity
Examination
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs:
- A high arch
- An area of maximum tenderness on the bottom of your foot, just in front of your heel bone
- Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down
- Limited “up” motion of your ankle
Tests
Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem.
X-rays
X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray.
Other Imaging Tests
Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Treatment
Nonsurgical Treatment
More than 90% of patients with plantar fasciitis will improve within 10 months of starting simple treatment methods.
Rest. Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics).
Ice. Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
Nonsteroidal anti-inflammatory medication. Drugs such as ibuprofen or naproxen reduce pain and inflammation. Using the medication for more than 1 month should be reviewed with your primary care doctor.
Exercise. Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is the most effective way to relieve the pain that comes with this condition.
- Calf stretch
Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch.
- Plantar fascia stretch
This stretch is performed in the seated position. Cross your affected foot over the knee of your other leg. Grasp the toes of your painful foot and slowly pull them toward you in a controlled fashion. If it is difficult to reach your foot, wrap a towel around your big toe to help pull your toes toward you. Place your other hand along the plantar fascia. The fascia should feel like a tight band along the bottom of your foot when stretched. Hold the stretch for 10 seconds. Repeat it 20 times for each foot. This exercise is best done in the morning before standing or walking.
Cortisone injections. Cortisone, a type of steroid, is a powerful anti-inflammatory medication. It can be injected into the plantar fascia to reduce inflammation and pain. Your doctor may limit your injections. Multiple steroid injections can cause the plantar fascia to rupture (tear), which can lead to a flat foot and chronic pain.
Soft heel pads can provide extra support.
Supportive shoes and orthotics. Shoes with thick soles and extra cushioning can reduce pain with standing and walking. As you step and your heel strikes the ground, a significant amount of tension is placed on the fascia, which causes microtrauma (tiny tears in the tissue). A cushioned shoe or insert reduces this tension and the microtrauma that occurs with every step. Soft silicone heel pads are inexpensive and work by elevating and cushioning your heel. Pre-made or custom orthotics (shoe inserts) are also helpful.
Night splints. Most people sleep with their feet pointed down. This relaxes the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be difficult to sleep with, a night splint is very effective and does not have to be used once the pain is gone.
Physical therapy. Your doctor may suggest that you work with a physical therapist on an exercise program that focuses on stretching your calf muscles and plantar fascia. In addition to exercises like the ones mentioned above, a physical therapy program may involve specialized ice treatments, massage, and medication to decrease inflammation around the plantar fascia.
Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged plantar fascia tissue. ESWT has not shown consistent results and, therefore, is not commonly performed.
ESWT is noninvasive—it does not require a surgical incision. Because of the minimal risk involved, ESWT is sometimes tried before surgery is considered.
Surgical Treatment
Surgery is considered only after 12 months of aggressive nonsurgical treatment.
Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs.
Complication rates for gastrocnemius recession are low, but can include nerve damage.
Plantar fascia release. If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage.
Complications. The most common complications of release surgery include incomplete relief of pain and nerve damage.
Recovery. Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted.
Posterior Tibial Tendon Dysfunction
Posterior tibial tendon dysfunction is one of the most common problems of the foot and ankle. It occurs when the posterior tibial tendon becomes inflamed or torn. As a result, the tendon may not be able to provide stability and support for the arch of the foot, resulting in flatfoot.
Most patients can be treated without surgery, using orthotics and braces. If orthotics and braces do not provide relief, surgery can be an effective way to help with the pain. Surgery might be as simple as removing the inflamed tissue or repairing a simple tear. However, more often than not, surgery is very involved, and many patients will notice some limitation in activity after surgery.
The posterior tibial tendon is one of the most important tendons of the leg. A tendon attaches muscles to bones, and the posterior tibial tendon attaches the calf muscle to the bones on the inside of the foot. The main function of the tendon is to hold up the arch and support the foot when walking.
The posterior tibial tendon attaches the calf muscle to the bones on the inside of the foot.
Cause
An acute injury, such as from a fall, can tear the posterior tibial tendon or cause it to become inflamed. The tendon can also tear due to overuse. For example, people who do high-impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Once the tendon becomes inflamed or torn, the arch will slowly fall (collapse) over time.
Posterior tibial tendon dysfunction is more common in women and in people older than 40 years of age. Additional risk factors include obesity, diabetes, and hypertension.
Symptoms
- Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area.
- Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time.
- Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot.
The most common location of pain is along the course of the posterior tibial tendon (yellow line), which travels along the back and inside of the foot and ankle.
Examination
Medical History and Physical Examination
This patient has posterior tibial tendon dysfunction with a flatfoot deformity. (Left) The front of her foot points outward. (Right) The “too many toes” sign. Even the big toe can be seen from the back of this patient’s foot.
Your doctor will take a complete medical history and ask about your symptoms. During the foot and ankle examination, your doctor will check whether these signs are present.
- Swelling along the posterior tibial tendon. This swelling is from the lower leg to the inside of the foot and ankle.
- A change in the shape of the foot. The heel may be tilted outward and the arch will have collapsed.
- “Too many toes” sign. When looking at the heel from the back of the patient, usually only the fifth toe and half of the fourth toe are seen. In a flatfoot deformity, more of the little toe can be seen.
This patient is able to perform a single limb heel rise on the right leg.
- “Single limb heel rise” test. Being able to stand on one leg and come up on “tiptoes” requires a healthy posterior tibial tendon. When a patient cannot stand on one leg and raise the heel, it suggests a problem with the posterior tibial tendon.
- Limited flexibility. The doctor may try to move the foot from side to side. The treatment plan for posterior tibial tendon tears varies depending on the flexibility of the foot. If there is no motion or if it is limited, there will need to be a different treatment than with a flexible foot.
- The range of motion of the ankle is affected. Upward motion of the ankle (dorsiflexion) can be limited in flatfoot. The limited motion is tied to tightness of the calf muscles.
Imaging Tests
Other tests which may help your doctor confirm your diagnosis include:
X-rays. These imaging tests provide detailed pictures of dense structures, like bone. They are useful to detect arthritis. If surgery is needed, they help the doctor make measurements to determine what surgery would most helpful.
(Top) An x-ray of a normal foot. Note that the lines are parallel, indicating a normal arch. (Bottom) In this x-ray the lines diverge, which is consistent with flatfoot deformity.
Magnetic resonance imaging (MRI). These studies can create images of soft tissues like the tendons and muscles. An MRI may be ordered if the diagnosis is in doubt.
Computerized tomography scan (CT Scan). These scans are more detailed than x-rays. They create cross-section images of the foot and ankle. Because arthritis of the back of the foot has similar symptoms to posterior tibial tendon dysfunction, a CT scan may be ordered to look for arthritis.
Ultrasound. An ultrasound uses high-frequency sound waves that echo off the body. This creates a picture of the bone and tissue. Sometimes more information is needed to make a diagnosis. An ultrasound can be ordered to show the posterior tibial tendon.
Nonsurgical Treatment
Symptoms will be relieved in most patients with appropriate nonsurgical treatment. Pain may last longer than 3 months even with early treatment. For patients who have had pain for many months, it is not uncommon for the pain to last another 6 months after treatment starts.
Rest
Decreasing or even stopping activities that worsen the pain is the first step. Switching to low-impact exercise is helpful. Biking, elliptical machines, or swimming do not put a large impact load on the foot, and are generally tolerated by most patients.
Ice
Apply cold packs on the most painful area of the posterior tibial tendon for 20 minutes at a time, 3 or 4 times a day to keep down swelling. Do not apply ice directly to the skin. Placing ice over the tendon immediately after completing an exercise helps to decrease the inflammation around the tendon.
Nonsteroidal Anti-inflammatory Medication
Drugs, such as ibuprofen or naproxen, reduce pain and inflammation. Taking such medications about a half of an hour before an exercise activity helps to limit inflammation around the tendon. The thickening of the tendon that is present is degenerated tendon. It will not go away with medication. Talk with your primary care doctor if the medication is used for more than 1 month.
Immobilization
A short leg cast or walking boot may be used for 6 to 8 weeks. This allows the tendon to rest and the swelling to go down. However, a cast causes the other muscles of the leg to atrophy (decrease in strength) and thus is only used if no other conservative treatment works.
Orthotics
Most people can be helped with orthotics and braces. An orthotic is a shoe insert. It is the most common nonsurgical treatment for a flatfoot. An over-the-counter orthotic may be enough for patients with a mild change in the shape of the foot. A custom orthotic is required in patients who have moderate to severe changes in the shape of the foot. The custom orthotic is more costly, but it allows the doctor to better control the position the foot.
Braces
A lace-up ankle brace may help mild to moderate flatfoot. The brace would support the joints of the back of the foot and take tension off of the tendon. A custom-molded leather brace is needed in severe flatfoot that is stiff or arthritic. The brace can help some patients avoid surgery.
Physical Therapy
Physical therapy that strengthens the tendon can help patients with mild to moderate disease of the posterior tibial tendon.
Steroid Injection
Cortisone is a very powerful anti-inflammatory medicine that your doctor may consider injecting around the tendon. A cortisone injection into the posterior tibial tendon is not normally done. It carries a risk of tendon rupture. Discuss this risk with your doctor before getting an injection.
Surgical Treatment
Surgery should only be done if the pain does not get better after 6 months of appropriate treatment. The type of surgery depends on where tendonitis is located and how much the tendon is damaged. Surgical reconstruction can be extremely complex. The following is a list of the more commonly used operations. Additional procedures may also be required.
Gastrocnemius Recession or Lengthening of the Achilles Tendon
This is a surgical lengthening of the calf muscles. It is useful in patients who have limited ability to move the ankle up. This surgery can help prevent flatfoot from returning, but does create some weakness with pushing off and climbing stairs. Complication rates are low but can include nerve damage and weakness. This surgery is typically performed together with other techniques for treating flatfoot.
Tenosynovectomy (Cleaning the Tendon)
This surgery is used when there is very mild disease, the shape of the foot has not changed, and there is pain and swelling over the tendon. The surgeon will clean away and remove the inflamed tissue (synovium) surrounding the tendon. This can be performed alone or in addition to other procedures. The main risk of this surgery is that the tendon may continue to degenerate and the pain may return.
Tendon Transfer
Tendon transfer can be done in flexible flatfoot to recreate the function of the damaged posterior tibial tendon. In this procedure, the diseased posterior tibial tendon is removed and replaced with another tendon from the foot, or, if the disease is not too significant in the posterior tibial tendon, the transferred tendon is attached to the preserved (not removed) posterior tibial tendon.
One of two possible tendons are commonly used to replace the posterior tibial tendon. One tendon helps the big toe point down and the other one helps the little toes move down. After the transfer, the toes will still be able to move and most patients will not notice a change in how they walk.
Although the transferred tendon can substitute for the posterior tibial tendon, the foot still is not normal. Some people may not be able to run or return to competitive sports after surgery. Patients who need tendon transfer surgery are typically not able to participate in many sports activities before surgery because of pain and tendon disease.
Osteotomy (Cutting and Shifting Bones)
An osteotomy can change the shape of a flexible flatfoot to recreate a more “normal” arch shape. One or two bone cuts may be required, typically of the heel bone (calcaneus).
If flatfoot is severe, a bone graft may be needed. The bone graft will lengthen the outside of the foot. Other bones in the middle of the foot also may be involved. They may be cut or fused to help support the arch and prevent the flatfoot from returning. Screws or plates hold the bones in places while they heal.
X-ray of a foot as viewed from the side in a patient with a more severe deformity. This patient required fusion of the middle of the foot in addition to a tendon transfer and cut in the heel bone.
Fusion
Sometimes flatfoot is stiff or there is also arthritis in the back of the foot. In these cases, the foot will not be flexible enough to be treated successfully with bone cuts and tendon transfers. Fusion (arthrodesis) of a joint or joints in the back of the foot is used to realign the foot and make it more “normal” shaped and remove any arthritis. Fusion involves removing any remaining cartilage in the joint. Over time, this lets the body “glue” the joints together so that they become one large bone without a joint, which eliminates joint pain. Screws or plates hold the bones in places while they heal.
This x-ray shows a very stiff flatfoot deformity. A fusion of the three joints in the back of the foot is required and can successfully recreate the arch and allow restoration of function.
Side-to-side motion is lost after this operation. Patients who typically need this surgery do not have a lot of motion and will see an improvement in the way they walk. The pain they may experience on the outside of the ankle joint will be gone due to permanent realignment of the foot. The up and down motion of the ankle is not greatly affected. With any fusion, the body may fail to “glue” the bones together. This may require another operation.
Complications
The most common complication is that pain is not completely relieved. Nonunion (failure of the body to “glue” the bones together) can be a complication with both osteotomies and fusions. Wound infection is a possible complication, as well.
Surgical Outcome
Most patients have good results from surgery. The main factors that determine surgical outcome are the amount of motion possible before surgery and the severity of the flatfoot. The more severe the problem, the longer the recovery time and the less likely a patient will be able to return to sports. In many patients, it may be 12 months before there is any great improvement in pain.
Rheumatoid Arthritis of the Foot and Ankle
Rheumatoid arthritis is a chronic disease that attacks multiple joints throughout the body. It most often starts in the small joints of the hands and feet, and usually affects the same joints on both sides of the body.
More than 90% of people with rheumatoid arthritis (RA) develop symptoms in the foot and ankle over the course of the disease.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In RA, the defenses that protect the body from infection instead damage normal tissue (such as cartilage and ligaments) and soften bone.
How It Happens
The joints of your body are covered with a lining — called synovium — that lubricates the joint and makes it easier to move. Rheumatoid arthritis causes an overactivity of this lining. It swells and becomes inflamed, destroying the joint, as well as the ligaments and other tissues that support it. Weakened ligaments can cause joint deformities — such as claw toe or hammer toe. Softening of the bone (osteopenia) can result in stress fractures and collapse of bone.
Rheumatoid arthritis is not an isolated disease of the bones and joints. It affects tissues throughout the body, causing damage to the blood vessels, nerves, and tendons. Deformities of the hands and feet are the more obvious signs of RA. In about 20% of patients, foot and ankle symptoms are the first signs of the disease.
In RA, the lining of the joint swells and becomes inflamed. This slowly destroys the joint.
Statistics
Rheumatoid arthritis affects approximately 1% of the population. Women are affected more often than men, with a ratio of up to 3 to 1. Symptoms most commonly develop between the ages of 40 and 60.
Cause
The exact cause of RA is not known. There may be a genetic reason — some people may be more likely to develop the disease because of family heredity. However, doctors suspect that it takes a chemical or environmental “trigger” to activate the disease in people who genetically inherit RA.
Symptoms
The most common symptoms are pain, swelling, and stiffness. Unlike osteoarthritis, which typically affects one specific joint, symptoms of RA usually appear in both feet, affecting the same joints on each foot.
Anatomy of the foot and ankle.
Ankle
Difficulty with inclines (ramps) and stairs are the early signs of ankle involvement. As the disease progresses, simple walking and standing can become painful.
Hindfoot (Heel Region of the Foot)
The main function of the hindfoot is to perform the side-to-side motion of the foot. Difficulty walking on uneven ground, grass, or gravel are the initial signs. Pain is common just beneath the fibula (the smaller lower leg bone) on the outside of the foot.
As the disease progresses, the alignment of the foot may shift as the bones move out of their normal positions. This can result in a flatfoot deformity. Pain and discomfort may be felt along the posterior tibial tendon (main tendon that supports the arch) on the inside of the ankle, or on the outside of the ankle beneath the fibula.
Midfoot (Top of the Foot)
With RA, the ligaments that support the midfoot become weakened and the arch collapses. With loss of the arch, the foot commonly collapses and the front of the foot points outward. RA also damages the cartilage, causing arthritic pain that is present with or without shoes. Over time, the shape of the foot can change because the structures that support it degenerate. This can create a large bony prominence (bump) on the arch. All of these changes in the shape of the foot can make it very difficult to wear shoes.
This x-ray shows signs of RA of the midfoot. Note that the front of the foot points outward and there is a large bump on the inside and bottom of the foot.
Forefoot (Toes and Ball of the Foot)
The changes that occur to the front of the foot are unique to patients with RA. These problems include bunions, claw toes, and pain under the ball of the foot (metatarsalgia). Although, each individual deformity is common, it is the combination of deformities that compounds the problem.
People with RA can experience a combination of common foot problems, such as bunions and clawtoe.
The bunion is typically severe and the big toe commonly crosses over the second toe.
There can also be very painful bumps on the ball of the foot, creating calluses. The bumps develop when bones in the middle of the foot (midfoot) are pushed down from joint dislocations in the toes. The dislocations of the lesser toes (toes two through five) cause them to become very prominent on the top of the foot. This creates clawtoes and makes it very difficult to wear shoes. In severe situations, ulcers can form from the abnormal pressure.
Severe claw toes can become fixed and rigid. They do not move when in a shoe. The extra pressure from the top of the shoe can cause severe pain and can damage the skin.
Examination
Medical History and Physical Examination
After listening to your symptoms and discussing your general health and medical history, your doctor will examine your foot and ankle.
Skin. The location of callouses indicate areas of abnormal pressure on the foot. The most common location is on the ball of the foot (the underside of the forefoot). If the middle of the foot is involved, there may be a large prominence on the inside and bottom of the foot. This can cause callouses.
Foot shape. Your doctor will look for specific deformities, such as bunions, claw toes, and flat feet.
Flexibility. In the early stages of RA, the joints will typically still have movement. As arthritis progresses and there is a total loss of cartilage, the joints become very stiff. Whether there is motion within the joints will influence treatment options.
Tenderness to pressure. Although applying pressure to an already sensitive foot can be very uncomfortable, it is critical that your doctor identify the areas of the foot and ankle that are causing the pain. By applying gentle pressure at specific joints your doctor can determine which joints have symptoms and need treatment. The areas on the x-ray that look abnormal are not always the same ones that are causing the pain.
Imaging Tests
Other tests that your doctor may order to help confirm your diagnosis include:
X-rays. This test creates images of dense structures, like bone. It will show your doctor the position of the bones. The x-rays can be used by your doctor to make measurements of the alignment of the bones and joint spaces, which will help your doctor determine what surgery would best.
Computerized tomography (CT) scan. When the deformity is severe, the shape of the foot can be abnormal enough to make it difficult to determine which joints have been affected and the extent of the disease. CT scans allow your doctor to more closely examine each joint for the presence of arthritis.
Magnetic resonance imaging (MRI) scan. An MRI scan will show the soft tissues, including the ligaments and tendons. Your doctor can assess whether the tendon is inflamed (tendonitis) or torn (ruptured).
Rheumatology Referral
Your doctor may refer you to a rheumatologist if he or she suspects RA. Although your symptoms and the results from a physical examination and tests may be consistent with RA, a rheumatologist will be able to determine the specific diagnosis. There are other less common types of inflammatory arthritis that will be considered.
Nonsurgical Treatment
Although there is no cure for RA, there are many treatment options available to help people manage pain, stay active, and live fulfilling lives.
Rheumatoid arthritis is often treated by a team of healthcare professionals. These professionals may include rheumatologists, physical and occupational therapists, social workers, rehabilitation specialists, and orthopaedic surgeons.
Although orthopaedic treatment may relieve symptoms, it will not stop the progression of the disease. Specific medicines called disease-modifying anti-rheumatic drugs are designed to stop the immune system from destroying the joints. The appropriate use of these medications is directed by a rheumatologist.
Orthopaedic treatment of RA depends on the location of the pain and the extent of cartilage damage. Many patients will have some symptom relief with appropriate nonsurgical treatment.
Rest
Limiting or stopping activities that make the pain worse is the first step in minimizing the pain. Biking, elliptical training machines, or swimming are exercise activities that allow patients to maintain their health without placing a large impact load on the foot.
Ice
Placing ice on the most painful area of the foot for 20 minutes is effective. This can be done 3 or 4 times a day. Ice application is best done right after you are done with a physical activity. Do not apply ice directly to your skin.
Nonsteroidal Anti-inflammatory Medication
Drugs, such as ibuprofen or naproxen, reduce pain and inflammation. In patients with RA, the use of these types of medications should be reviewed with your rheumatologist or medical doctor.
Orthotics
An orthotic (shoe insert) is a very effective tool to minimize the pressure from prominent bones in the foot. The orthotic will not be able to correct the shape of your foot. The primary goal is to minimize the pressure and decrease the pain and callous formation. This is more effective for deformity in the front and middle of the foot.
A custom-molded leather brace can be effective in minimizing the pain and discomfort from ankle and hindfoot arthritis.
For people with RA, hard or rigid orthotics generally cause too much pressure on the bone prominences, creating more pain. A custom orthotic is generally made of softer material and relieves pressure on the foot.
Braces
A lace-up ankle brace can be an effective treatment for mild to moderate pain in the back of the foot and the ankle. The brace supports the joints of the back of the foot and ankle. In patients with a severe flatfoot or a very stiff arthritic ankle, a custom-molded plastic or leather brace is needed. The brace can be a very effective device for some patients, allowing them to avoid surgery.
Steroid Injection
An injection of cortisone into the affected joint can help in the early stages of the disease. In many cases, a rheumatologist or medical doctor may also perform these injections. The steroid helps to reduce inflammation within the joint. The steroid injection is normally a temporary measure and will not stop the progression of the disease.
Surgical Treatment
Your doctor may recommend surgery depending upon the extent of cartilage damage and your response to nonsurgical options.
Fusion. Fusion of the affected joints is the most common type of surgery performed for RA. Fusion takes the two bones that form a joint and fuses them together to make one bone.
During the surgery, the joints are exposed and the remaining cartilage is removed. The two bones are then held together with screws or a combination of screws and plates. This prevents the bones from moving. During the healing process, the body grows new bone between the bones in these joints.
Because the joint is no longer intact, this surgery does limit joint motion. Limited joint motion may not be felt by the patient, depending on the joints fused. The midfoot joints often do not have much motion to begin with, and fusing them does not create increased stiffness. The ankle joint normally does have a lot of motion, and fusing it will be noticeable to the patient. By limiting motion, fusion reduces the pain.
Fusion can be a successful technique. However, because patients with RA also show damaged cartilage and loose ligaments, the success rate of this type of surgery is lower in patients with RA than in patients without RA. The use of newer generation medication can slow the progression of the disease and impact the type of surgeries that can be performed successfully.
Other surgeries. The front of the foot is where there are more surgical options for some patients. Surgeons can now perform joint sparing operations to correct the bunion and hammertoes in some patients. Your surgeon will review the most appropriate options for your case.
Ankle
Ankle fusion and total ankle replacement are the two primary surgical options for treating RA of the ankle. Both treatment options can be successful in minimizing the pain and discomfort in the ankle. The appropriate surgery is based upon multiple factors and is individualized for every patient.
The patient shown in these x-rays had arthritis of the hindfoot. It was treated by fusing all three joints of the hindfoot (triple fusion). An ankle replacement was also done in order to improve mobility and avoid the severe stiffness that would result from another ankle fusion. The ankle replacement implants can be seen here from the front and the side.
Patients with severe involvement of other joints around the heel or patients who have previously undergone a fusion on the other leg, may be more suited for ankle replacement. In addition, patients who have fusions within the same foot may be more suited for an ankle replacement.
Newer generation ankle replacement implants have shown promising early results. Ankle replacement implants have not yet been shown to be as long-lasting as those for the hip or knee, due to the fact that the newer generation of implants have not been available long enough to determine how long they will last.
These x-rays show an ankle fusion from the front and the side. The number and placement of screws and the use of a plate are dependent upon the surgeon’s technique.
Following ankle fusion, there is a loss of the up and down motion of the ankle. The up and down motion is transferred to the joints near the ankle. This creates a potential for pain in those joints, and possibly arthritis.
Patients are able to walk in shoes on flat, level ground without much difficulty after an ankle fusion, despite the loss of ankle motion. The joints in the foot next to the ankle joint allow for motion similar to the ankle joint, and help patients with fused ankle joints walk more normally.
Over time, the increased stress that is placed on the rest of the foot after an ankle fusion can lead to arthritis of the joints surrounding the ankle. This patient had pain in the subtalar joint (arrow) and required an additional fusion of that joint to minimize the pain. Increased stress on other joints is the most concerning problem following ankle fusion.
Hindfoot (Heel Region of the Foot)
A fusion of the affected joints of the hindfoot is the most common surgery used to treat patients with flatfoot or arthritis of the hindfoot. A triple arthrodesis is a fusion that involves all three joints in the back of the foot. Occasionally, the joint on the outside of the foot is not fused if there is minimal to no involvement of that joint (this is at the surgeon’s discretion). This type of fusion eliminates the side-to-side motion of the foot, while preserving most of the up and down movement.
If RA is only in one joint, then a fusion of just that affected joint may be all that is needed.
(Left) In this x-ray, two of the three joints in the hindfoot have been fused. (Right) Just the subtalar joint is fused in this x-ray.
Any fusion of the hindfoot will limit side-to-side motion of the foot. This will affect walking on uneven ground, grass, or gravel. There is no method to replace the joints of the hindfoot.
Midfoot (Middle of the Foot)
Fusion is the most reliable surgical method to treat RA of the midfoot joints. If the shape of the foot is not normal, surgery is designed to help restore the arch and minimize the prominences on the foot.
There are joint replacement implants available for joints on the outside of the midfoot. This may preserve some midfoot motion. However, the use of these implants is at the surgeon’s discretion. These implants are not available for the joints on the inside of the midfoot.
Although the foot cannot be returned to a normal shape, the goals are to reduce pain in the foot and improve the potential for the patient to wear more normal shoes.
(Top) This x-ray shows RA of the midfoot that has collapsed the arch. (Bottom) The surgical reconstruction involved a fusion of the middle of the foot with plates and screws.
Forefoot (Toes and Ball of the Foot)
The choice of treatment for patients with a bunion or lesser toe deformities (hammer or claw toes) depends on a number of factors.
If the disease is very mild, joint-sparing procedures that preserve motion can be considered. The decision is dependent on the medication that the patient is taking and the amount of damaged cartilage that is present. A fusion of the great toe may be recommended despite that fact the bunion is very mild. If there is damage to the cartilage of the great toe joint, correcting the bunion will not minimize the arthritic pain.
If the RA has progressed and the lesser toes (two through five) have dislocated, a complex operation to minimize the pain and restore the shape of the foot may be recommended. The operation involves fusion of the big toe and removing a portion of bone of each of the metatarsals. This surgery removes the prominent bone on the bottom of the foot that is a source of the pain and allows the toes to re-align into a better position.
Occasionally, the lesser toe metatarsals can be preserved by shortening them to allow the toes to resume their position within the joints. This is not always possible, however, and the joint may have to be removed.
(Left) RA of the forefoot. The big toe is deviated and crosses over the second toe, a typical appearance of a bunion. The lesser toes (two through five) are dislocated, resulting in painful and severe claw toes. (Right) This x-ray taken immediately after fusion of the big toe shows that the prominent bones on the ball of the foot were removed and the claw toes were corrected. The pins hold the toes in place while the soft tissues heal. The pins are removed in the office after 4 to 6 weeks with minimal discomfort.
To fix the bend in the toes themselves, the surgeon may suggest cutting a tendon or removing a small portion of bone of the toes to allow them to straighten. Pins that stick out of the foot are temporarily required and will be removed in the office after healing takes place.
There are some newer implants available that can be buried within the toes, which avoid the need for pins sticking out of the foot. These implants may not work if the bone is soft, or if significant destruction of the joints has occurred.
This operation puts a lot of stress on the blood vessels and skin of the foot. In severe cases, the toes may not survive the operation and may require amputation of a portion or the entire toe. This operation can provide the patient with a high level of function and the ability to enjoy a wider variety of shoewear.
Preparing for Surgery
Many of the medications that help with RA also affect the ability of the body to heal wounds and fight infection. Your surgeon will work with your rheumatologist or medical doctor to review which of your medications will need to be stopped prior to surgery. Once the wounds are healed, the medication is typically resumed.
This period of time can be very difficult for patients with other areas of the body that are affected by RA. Many fusions require at least 6 weeks of time where no pressure can be placed on the foot. Making appropriate preparations to ensure you have help at home is crucial for success after surgery.
Stiff Big Toe (Hallux Rigidus)
The most common site of arthritis in the foot is at the base of the big toe. This joint is called the metatarsophalangeal, or MTP joint. It’s important because it has to bend every time you take a step. If the joint starts to stiffen, walking can become painful and difficult.
In the MTP joint, as in any joint, the ends of the bones are covered by a smooth articular cartilage. If wear-and-tear or injury damage the articular cartilage, the raw bone ends can rub together. A bone spur, or overgrowth, may develop on the top of the bone. This overgrowth can prevent the toe from bending as much as it needs to when you walk. The result is a stiff big toe, or hallux rigidus.
Hallux rigidus usually develops in adults between the ages of 30 and 60 years. No one knows why it appears in some people and not others. It may result from an injury to the toe that damages the articular cartilage or from differences in foot anatomy that increase stress on the joint.
- Pain in the joint when you are active, especially as you push-off on the toes when you walk
- Swelling around the joint
- A bump, like a bunion or callus, that develops on the top of the foot
- Stiffness in the great toe and an inability to bend it up or down
Diagnosis
If you find it difficult to bend your toe up and down or find that you are walking on the outside of your foot because of pain in the toe, see your doctor right away. Hallux rigidus is easier to treat when the condition is caught early. If you wait until you see a bony bump on the top of your foot, the bone spurs will have already developed and the condition will be more difficult to treat.
Your physician will examine your foot and look for evidence of bone spurs. He or she may move the toe around to see how much motion is possible without pain. X-rays will show the location and size of any bone spurs, as well as the degree of degeneration in the joint space and cartilage.
Treatment
Nonsurgical Treatment
Pain relievers and anti-inflammatory medications such as ibuprofen may help reduce the swelling and ease the pain. Applying ice packs or taking contrast baths (described below) may also help reduce inflammation and control symptoms for a short period of time. But they aren’t enough to stop the condition from progressing. Wearing a shoe with a large toe box will reduce the pressure on the toe, and you will probably have to give up wearing high heels. Your doctor may recommend that you get a stiff-soled shoe with a rocker or roller bottom design and possibly even a steel shank or metal brace in the sole. This type of shoe supports the foot when you walk and reduces the amount of bend in the big toe.
A contrast bath uses alternating cold and hot water to reduce inflammation. You’ll need two buckets, one with water as cold as you can tolerate and the other with water as warm as you can tolerate. Immerse your foot in the cold water for 30 seconds, then immediately place it in the hot water for 30 seconds. Continue to alternate between cold and hot for five minutes, ending in the cold water. You can do contrast baths up to three times a day. However, be careful to avoid extreme temperatures in the water, especially if your feet aren’t very sensitive to heat or cold.
Surgical Treatment
- Cheilectomy (kI-lek’-toe-me)This surgery is usually recommended when damage is mild or moderate. It involves removing the bone spurs as well as a portion of the foot bone, so the toe has more room to bend. The incision is made on the top of the foot. The toe and the operative site may remain swollen for several months after the operation, and you will have to wear a wooden-soled sandal for at least two weeks after the surgery. But most patients do experience long-term relief.
- Arthrodesis (are-throw-dee’-sis)Fusing the bones together (arthrodesis) is often recommended when the damage to the cartilage is severe. The damaged cartilage is removed and pins, screws, or a plate are used to fix the joint in a permanent position. Gradually, the bones grow together. This type of surgery means that you will not be able to bend the toe at all. However, it is the most reliable way to reduce pain in these severe cases.For the first six weeks after surgery, you will have to wear a cast and then use crutches for about another six weeks. You won’t be able to wear high heels, and you may need to wear a shoe with a rocker-type sole.
- Arthroplasty (are-throw-plas’-tee)Older patients who place few functional demands on the feet may be candidates for joint replacement surgery. The joint surfaces are removed and an artificial joint is implanted. This procedure may relieve pain and preserve joint motion.
Tarsal Coalition
A tarsal coalition is an abnormal connection of two or more bones in the foot. The bones affected — called tarsal bones — are located toward the back of the foot and in the heel, and the connection of the bones can result in a severe, rigid flatfoot.
Although tarsal coalition is often present at birth, children typically do not show signs of the disorder until early adolescence. The foot may become stiff and painful, and everyday physical activities are often difficult.
For many children with tarsal coalition, symptoms are relieved with simple treatments, such as orthotics and physical therapy. If a child has severe symptoms that do not respond to simple treatments and continue to interfere with their daily activities, surgery may be recommended.
The calcaneus, talus, and navicular bones are those most often affected by tarsal coalition.
The bones of the feet are commonly divided into three parts: the hindfoot, midfoot, and forefoot. Seven bones — called tarsals — compose the hindfoot and midfoot. Of these bones, the calcaneus, talus, and navicular are most commonly involved in tarsal coalition.
Description
A tarsal coalition occurs when two bones grow into one another, connected by a bridge of bone, cartilage, or strong, fibrous tissue. These bridges are often referred to as “bars” and they can cover just a small amount of the joint space between the bones, or a large portion of the space.
The two most common sites of tarsal coalition are between the calcaneus and navicular bones, or between the talus and calcaneus bones. However, other joints can also be affected.
In this anatomy model of the foot, surgical instruments point out a coalition bridge between the calcaneus and navicular bones.
It is estimated that one out of every 100 people may have a tarsal coalition. In about 50% of cases, both feet are affected. The exact incidence of the disorder is hard to determine because many coalitions never cause noticeable symptoms.
In most people, the condition begins before birth. It is caused by a gene mutation that affects the cells that produce the tarsal bones. Although the coalition forms before birth, its presence is often not discovered until late childhood or adolescence.
This is because babies’ feet contain a higher percentage of soft, growing cartilage. As a child grows, this cartilage mineralizes (ossifies), resulting in hard, mature bone. If a coalition exists, it may harden, too, and fuse the growing bones together with a solid bridge of bone or fibrous tissue similar to a scar. The ossification of the coalition typically happens between ages 8 and 16, depending upon which bones are involved. As a result, the hindfoot stiffens, causing pain and other symptoms.
The stiffness and stress that tarsal coalitions produce may lead to arthritis over time.
(Left) An x-ray image of a healthy foot. (Right) An x-ray image that shows a large tarsal coalition that has fused the talus and navicular bones together.
Symptoms
Many tarsal coalitions are never discovered because they do not cause symptoms or any obvious foot deformity. When symptoms do occur, they may include:
- Stiff, painful feet. The pain usually occurs below the ankle around the middle or back half of the foot.
- A rigid, flat foot that makes it difficult to walk on uneven surfaces. To accommodate for the foot’s lack of motion, the patient may roll the ankle more than normal, which may result in recurrent ankle sprains.
- Increased pain or a limp with higher levels of activity.
Examination
Medical History and Physical Examination
After discussing your symptoms and general health history, your doctor will do a complete examination of your foot and ankle, which will include checking your foot flexibility and gait. Patients with tarsal coalitions may have a flat arch that does not fully correct when pushing up on the toes and raising the heel.
(Left) A side view of a young person with flat foot. (Right) The feet remain flat when performing a toe raise.
Imaging Tests
To accurately diagnose the number, location and extent of the coalition(s), your doctor will order images of your foot and ankle.
- X-rays. These tests provide clear images of bone. Many coalitions are visible on x-rays.
- Computed tomography (CT) scans. The images produced with computed tomography provide greater detail of the bones. CT scans are the gold standard for imaging tarsal coalitions because they can show more subtle bars that may be missed with plain x-rays.
This CT image displays a cross-section view of the hindfoot and shows a large coalition fusing the talus and calcaneus bones.
Magnetic resonance (MRI) scans. These imaging tests provide detailed pictures that include soft tissues. Your doctor may order this test to look for irregular bars formed from cartilage or fibrous tissue.
Treatment
Tarsal coalitions only require treatment if they are causing symptoms.
Nonsurgical Treatment
- Rest. Taking a break from high-impact activity for a period time — 3 to 6 weeks — can reduce stress on the tarsal bones and relieve pain.
- Orthotics. Arch supports, shoe inserts like heel cups and wedges, and other types of orthotics may be recommended to help stabilize the foot and relieve pain.
- Temporary boot or cast. These options can immobilize the foot and take stress off of the tarsal bones.
- Injections. Steroid medications may be used in conjunction with other nonsurgical options to provide temporary pain relief.
Surgical Treatment
When nonsurgical treatments are not effective at easing pain or improving function, your doctor may consider surgery.
The surgical procedure your doctor recommends will depend on the size and location of the coalition, as well as whether the joints between the bones show signs of arthritis.
- Resection. In this procedure, the coalition is removed and replaced with muscle or fatty tissue from another area of the body. This is the most common surgery for tarsal coalition because it preserves normal foot motion and successfully relieves symptoms in most patients who do not have signs of arthritis.
These CT cross-section images show a patient with coalitions between the calcaneus and talus in both feet. At the time of this scan, the coalition on the left foot had been resected, and the right foot was awaiting the procedure.
- Fusion. Larger, more severe coalitions that cause significant deformity and also involve arthritis may be treated with joint fusion. The goal of fusion is to limit movement of painful joints and place the bones in the proper position. In fusion for tarsal coalition, the bones may be held in place with large screws, pins, or screw-and-plate devices.
Depending upon the type and location of your surgery, a cast will be required for a period of time to protect the surgical site and prevent you from putting weight on the foot. Casts are typically replaced with walking boots, and your doctor may recommend physical therapy exercises to begin restoring range of motion and strength.
Your doctor will determine when it is safe for you to begin putting weight on your foot. Arch supports or orthotics may also be helpful in stabilizing the joint, even after surgery.
Although it may take several months to fully recover, most patients have pain relief and improved motion after surgery.
Bunion Surgery
Most people with bunions find pain relief with simple treatments to reduce pressure on the big toe, such as wearing wider shoes or using pads in their shoes. However, if these measures do not relieve your symptoms, your doctor may recommend bunion surgery.
There are different types of surgeries to correct a bunion. Bringing the big toe back to its correct position may involve realigning bone, ligaments, tendons, and nerves.
In general, if your bunion is not painful, you do not need surgery. Although bunions often get bigger over time, doctors do not recommend surgery to prevent bunions from worsening. Many people can slow the progression of a bunion with proper shoes and other preventive care, and the bunion never causes pain or other problems.
It is also important to note that bunion surgery should not be done for cosmetic reasons. After surgery, it is possible for ongoing pain to develop in the affected toe — even though there was no bunion pain prior to surgery.
Good candidates for bunion surgery commonly have:
- Significant foot pain that limits their everyday activities, including walking and wearing reasonable shoes. They may find it hard to walk more than a few blocks (even in athletic shoes) without significant pain.
- Chronic big toe inflammation and swelling that does not improve with rest or medications
- Toe deformity—a drifting in of the big toe toward the smaller toes, creating the potential for the toes to cross over each other.
- Toe stiffness—the inability to bend and straighten the big toe
- Failure to obtain pain relief with changes in footwear
- Failure to obtain pain relief from nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen. The effectiveness of NSAIDs in controlling toe pain varies greatly from person to person.
(Left) A bunion that has progressed to deformity with the big toe crossing over the second toe. (Right) An x-ray of the same bunion shows how far out of alignment the bones are.
Deciding to Have Bunion Surgery
After bunion surgery, most patients have less foot pain and are better able to participate in everyday activities.
Although many bunion procedures are done on a same-day basis with no hospital stay, a long recovery period is common. It often takes up to 6 months for full recovery, with follow-up visits to your doctor sometimes necessary for up to a year.
It is very important to have realistic expectations about bunion surgery. For example, bunion surgery may not allow you to wear a smaller shoe size or narrow, pointed shoes. In fact, you may need to restrict the types of shoes you wear for the rest of your life.
Surgical Procedures
In general, the common goals of most bunion surgeries include:
- Realigning the metatarsophalangeal (MTP) joint at the base of the big toe
- Relieving pain
- Correcting the deformity of the bones making up the toe and foot
Because bunions vary in shape and size, there are different surgical procedures performed to correct them. In most cases, bunion surgery includes correcting the alignment of the bone and repairing the soft tissues around the big toe.
Your doctor will talk with you about the type of surgery that will best correct your bunion.
Repairing the Tendons and Ligaments Around the Big Toe
In some cases, the soft tissues around the big toe may be too tight on one side and too loose on the other. This creates an imbalance that causes the big toe to drift toward the other toes.
Surgery can shorten the loose tissues and lengthen the tight ones. This is rarely done without some type of alignment of the bone, called an osteotomy. In the majority of cases, soft tissue correction is just one portion of the entire bunion corrective procedure.
Osteotomy
In an osteotomy, your doctor makes small cuts in the bones to realign the joint. After cutting the bone, your doctor fixes this new break with pins, screws, or plates. The bones are now straighter, and the joint is balanced.
Osteotomies may be performed in different places along the bone to correct the deformity. In some cases, in addition to cutting the bone, a small wedge of bone is removed to provide enough correction to straighten the toe.
As discussed above, osteotomies are normally performed in combination with soft tissue procedures, as both are often necessary to maintain the big toe alignment.
X-rays taken from the top and the side of the foot show a bunion corrected with osteotomy.
Arthrodesis
In this procedure, your doctor removes the arthritic joint surfaces, then inserts screws, wires, or plates to hold the surfaces together until the bones heal. Arthrodesis is commonly used for patients who have severe bunions or severe arthritis, and for patients who have had previous unsuccessful bunion surgery.
The x-ray on the left shows severe arthritis of the MTP joint. After arthrodesis (shown on the right), the entire foot is realigned. An advantage of arthrodesis is that no additional procedures are necessary to correct the bunion.
Exostectomy
In this procedure, your doctor removes the bump from your toe joint. Exostectomy alone is seldom used to treat bunions because it does not realign the joint. Even when combined with soft tissue procedures, exostectomy rarely corrects the cause of the bunion.
Exostectomy is most often performed as one part of an entire corrective surgery that includes osteotomy, as well as soft-tissue procedures. If a doctor performs exostectomy without osteotomy, however, the bunion deformity often returns.
The x-ray on the left shows a mild bunion bump before exostectomy. After the procedure (right), the bump has been shaved but the toe deformity remains and is actually worse; the big toe drifts closer to the other toes and the metatarsal bone sticks out further.
Resection Arthroplasty
In this procedure, your doctor removes the damaged portion of the joint. This increases the space between the bones and creates a flexible “scar” joint. Resection arthroplasty is used mainly for patients who are elderly, have had previous unsuccessful bunion surgery, or have severe arthritis not amenable to an arthrodesis (see above). Because this procedure can change the push off power of the big toe, it is not often recommended.
This x-ray shows a failed resection arthroplasty. Although the damaged bone of the MTP joint was removed, scar tissue did not fill the space between the bones. The bone edges are still in contact. The photograph shows that without the needed scar tissue, the big toe is shortened. This makes it more difficult to push off while walking.
Preparing for Surgery
Medical Evaluation
Before your surgery, you may be asked to visit your family doctor for a complete physical examination. He or she will assess your health and identify any problems that could interfere with your surgery. If you have a heart or lung condition or a chronic illness you will need a preoperative medical clearance from your family doctor.
Medications
Tell your doctor about any medications you are taking. He or she will tell you which medications you can continue taking and which you should stop taking before surgery.
Tests
You may require several preoperative tests, including blood counts, a cardiogram, and a chest x-ray. You may also need to provide a urine sample.
To help plan your procedure, your doctor may order special foot x-rays. These x-rays should be taken in a standing, weight bearing position to ensure your doctor can clearly see the deformity in the foot. These x-rays assist your doctor in making decisions about where along the bone to perform an osteotomy in order to provide enough corrective power to straighten the toe.
Your Surgery
In planning your surgery, your doctor will consider several things, including how severe your bunion is, your age, your general health and activity level, and any other medical issues that may affect your recovery.
Almost all bunion surgery is done on an outpatient basis. You will most likely be asked to arrive at the hospital or surgical center 1 or 2 hours before your surgery.
Anesthesia
After admission, you will be evaluated by a member of the anesthesia team. Most bunion surgery is performed with anesthesia that numbs the area for surgery but does not put you to sleep.
- Local anesthesia. An ankle block numbs just your foot.
- Regional anesthesia. A popliteal block works for a longer period of time compared to an ankle block and numbs more of the leg. The numbing medicine is injected behind the knee.
- Spinal anesthesia. This injection will numb your body below your waist.
- General anesthesia. This form of anesthesia will put you to sleep.
The anesthesiologist will stay with you throughout the procedure to administer other medications, if necessary, and to make sure you are comfortable.
Procedure
Depending upon your bunion and the procedures you need, your doctor will make an incision along the inside of your big toe joint or on top of the joint. In some cases, more than one incision is needed to correct the bunion deformity.
This surgical photograph shows a saw cutting the bone to perform an osteotomy.
The surgical time varies depending on how much of your foot is malaligned. Surgery will take longer if your deformity is greater or if more than one osteotomy is required. Every bunion correction is a little bit different, and there is no reason to be concerned if your surgery takes more time.
Afterward, you will be moved to the recovery room. You will be ready to go home in an hour or two. Be sure to have someone with you to drive you home.
(Left) The bunion that was shown at the beginning of this article as it appeared immediately after surgery. (Right) An x-ray showing the bones in alignment after surgery. Osteotomies were performed on both bones; screws and plates hold the bones in place.
Complications
As with any surgical procedure, there are risks associated with bunion surgery. These occur infrequently and are usually treatable — although, in some cases, they may limit or extend your full recovery. Before your surgery, your doctor will discuss each of the risks with you and take specific measures to avoid complications.
The possible risks and complications of bunion surgery include:
- Infection
- Nerve injury
- Failure to relieve pain
- Failure of the bone to fully heal
- Stiffness of the big toe joint
- Recurrence of the bunion
Recovery at Home
The success of your surgery will depend in large part on how well you follow your doctor’s instructions at home during the first few weeks after surgery. You will see your doctor regularly for several months — occasionally up to a year — to make sure your foot heals properly.
Your doctor will apply your dressing in a specific way to keep the bones in correct position.
You will be discharged from the hospital with bandages holding your toe in its corrected position.
Because keeping your toe in position is essential for successful healing, it is very important to follow your doctor’s directions about dressing care. Do not disturb or change the dressing without talking to your doctor. Interfering with proper healing could cause a recurrence of the bunion.
Be sure to keep your wound and dressing dry. When you are showering or bathing, cover your foot with a plastic bag.
Your sutures will be removed about 2 weeks after surgery, but your foot will require continued support from dressings or a brace for 6 to 12 weeks.
Swelling
Keep your foot elevated as much as possible for the first few days after surgery, and apply ice as recommended by your doctor to relieve swelling and pain. Never apply ice directly on your skin. It is common to have some swelling in your foot from 6 months to a year after bunion surgery.
Bearing Weight
Your doctor will give you strict instructions about whether and when you can put weight on your foot. Depending upon the type of procedure you have, if you put weight on your foot too early or without proper support, the bones can shift and the bunion correction will be lost.
Some bunion procedures allow you to walk on your foot right after the surgery. In these cases, patients must use a special surgical shoe to protect the bunion correction.
Many bunion surgeries require a period of no weightbearing to ensure bone healing. Your doctor will apply dressings, a brace, or a cast to maintain the correct bone position. Crutches are usually used to avoid putting any weight on the foot. A newer device called a knee walker is a good alternative to crutches. It has four wheels and functions like a scooter. Instead of standing, you place the knee of your affected foot on a padded cushion and push yourself along using your healthy foot.
In addition to no weightbearing, driving may be restricted until the bones have healed properly — particularly if the surgery was performed on your right foot.
No matter what type of bunion surgery you have, it is very important to follow your doctor’s instructions about weightbearing. Do not put weight on your foot or stop using supportive devices until your doctor gives approval.
Physical Therapy and Exercise
Specific exercises will help restore your foot’s strength and range of motion after surgery. Your doctor or physical therapist may recommend exercises using a surgical band to strengthen your ankle or using marbles to restore motion in your toes.
Always start these exercises slowly and follow instructions from your doctor or physical therapist regarding repetitions.
Shoe Wear
It will take several months for your bones to fully heal. When you have completed the initial rehabilitation period, your doctor will advise you on shoewear. Athletic shoes or soft leather oxford type shoes will best protect the bunion correction until the bones have completely healed.
To help prevent your bunion from recurring, do not wear fashion shoes until your doctor allows it. Be aware that your doctor may recommend that you never return to wearing high-heeled shoes.
Avoiding Complications
Though uncommon, complications can occur following bunion surgery. During your recovery at home, contact your doctor if:
- Your dressing loosens, comes off, or gets wet.
- Your dressing is moistened with blood or drainage.
- You develop side effects from postoperative medications.
Also, call your doctor immediately if you notice any of the following warning signs of infection:
- Persistent fever
- Shaking chills
- Persistent warmth or redness around the dressing
- Increased or persistent pain, especially a “sunburn” type pain
- Significant swelling in the calf above the treated foot, especially if there is a “charley horse” pain behind the knee, or if your develop shortness of breath.
Outcomes
The majority of patients who undergo bunion surgery experience a reduction of foot pain, along with improvement in the alignment of their big toe. The length of your recovery will depend upon the surgical procedures that were performed, and how well you follow your doctor’s instructions.
Because a main cause of bunion deformity is a tight-fitting shoe, returning to that type of shoe can cause your bunion to return. Always follow your doctor’s recommendations for proper shoe fit.
Total Ankle Arthroplasty
What is total ankle arthroplasty?
Total ankle arthroplasty (TAA), also known as total ankle replacement, is a surgical procedure that orthopaedic foot and ankle surgeons use to treat ankle arthritis. Arthritic changes may be a result of normal wear and tear due to aging or from an injury such as a broken ankle or dislocation. Arthritis eventually leads to loss of cartilage, pain and/or deformity.
What are the goals of TAA?
The goal of TAA is to improve ankle motion so the patient has less pain during activity.
What signs indicate TAA may be needed?
TAA is considered in patients that experience ankle pain and decreased function from arthritis after trying conservative management. Conservative management includes anti-inflammatory medication, bracing, physical therapy, activity modification and pain medication. Patients with rheumatoid arthritis are usually good candidates for the ankle joint replacement. Other patients that should be considered are those that need but do not want a fusion-type procedure that would eliminate the motion at the ankle joint.
When should I avoid a TAA?
TAA is not suited for patients with significant deformity or dead bone in the talus, which is the bottom bone of the ankle joint. Prior or current infections of the ankle, significant lower extremity neuropathy, inadequate or absent leg muscle function, poor blood flow of the leg, or inadequate soft tissues are also signs that TAA should be avoided.
General Details of Procedure
TAA is performed either under general anesthetic or nerve block. A tourniquet is used at the time of surgery to control bleeding and improve visualization during the surgery. The ankle is approached from the front or the side depending on the type of implant being used. Bone is then cut, allowing for placement of the metal and plastic components that re-create the ankle joint. Sometimes the patient will have a tight calf muscle or tight Achilles tendon that needs to be lengthened to improve range of motion of the ankle. The wounds are then closed using stitches or staples, and a splint is applied. A period of non-weightbearing in either a cast or cast boot is necessary to allow the implants to heal in place.
Specific Technique
Either before or after the ankle replacement is put in place, the orthopaedic foot and ankle surgeon will determine if the calf muscle or Achilles is tight. A tight calf muscle or Achilles tendon is addressed with a lengthening procedure. This is important to improve motion after the surgery, as well as to take stress off the ankle replacement.
What happens after surgery?
Recovery from a total ankle replacement requires a period of non-weightbearing and immobilization. The procedure is usually
performed in an inpatient setting, with the patient spending one to several nights in the hospital. Strict elevation for many days after the procedure is necessary to control swelling and improve wound healing. After the surgical wounds are healed, some orthopaedic foot and ankle surgeons will allow the patient to start working on gentle range-of-motion activities even if they are non-weightbearing. Weightbearing usually begins a few weeks after surgery if X-rays show good healing.
Potential Complications
There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Fracture of bone on either side of the total ankle implant is the most common complication. Injury to tendons or nerves and blood vessels is also a possible complication of ankle replacement. Wound healing can be a problem in patients that smoke or have diabetes, or in patients that have rheumatoid arthritis. Another complication that is sometimes seen is the failure of the ankle implant to heal into the bone.
Frequently Asked Questions
There are two surgical approaches for treatment of arthritis: ankle fusion and total ankle replacement. Why should I consider an ankle replacement?
When motion of the ankle is preserved in a TAA, the surrounding joints are protected from increased wear. This helps preserve the surrounding joints from arthritis. It is usual for people with ankle fusions to have progressive arthritis in the surrounding joints in about 10 to 15 years.
The number of ankle replacements being performed is increasing dramatically. This is a result of improved outcomes. Newer implant designs and improved surgical techniques are helping patients be more active after a TAA than they were previously.
Who should I see to have a total ankle replacement?
An orthopaedic foot and ankle surgeon should be seen for management of ankle arthritis. Orthopaedic surgeons who specialize in foot and ankle surgery are specifically trained to perform ankle replacements as well as take care of any complications should they arise.
Lateral Ankle Ligament Reconstruction
What is the goal of lateral ankle ligament reconstruction (ALR)?
The goal of this surgery is to restore normal stability to the ankle. This should also fix a patient’s feeling that the ankle “gives way” and any pain that is associated with an unstable ankle.
What signs indicate surgery may be needed?
Surgery is considered when you have an unstable ankle that does not respond to nonsurgical treatment. Six months of nonsurgical treatment is often recommended before surgery. A physical examination will show that the ankle is unstable, and X-rays are sometimes used to help with the diagnosis.
When should I avoid surgery?
Your general health plays a role in any decision to have surgery. Patients with nerve or collagen diseases may not be helped by this type of surgery. Other diagnoses, including ankle joint arthritis, may require different surgeries that treat the bones and joints. Chronic pain may benefit most from nonsurgical management with a pain specialist. Surgery is not recommended for treatment of a single ankle sprain.
General Details of the Procedure
ALR is typically an outpatient surgery. It is most often done under general or regional anesthesia. Other surgeries may be performed at the same time. This commonly includes arthroscopic surgery of the ankle joint. At least one larger incision is required for the ligament reconstruction.
Several different techniques can be performed depending on the individual patient. One option is to repair the patient’s own existing ligaments with stitches. This repair is often made stronger by support from other tissues. This is referred to as the modified Bröstrom procedure. Another option is to use a tendon to replace the torn ligaments. This technique is similar to what is done in knee ligament reconstructions.
Specific Techniques
The modified Bröstrom procedure is the most commonly performed surgery for this problem. The surgeon begins by making a C- or J-shaped incision over the outside of the ankle. The ankle ligaments are identified if possible.They are then tightened using either stitches or anchors that are placed into one the bones of the ankle (the fibula bone). Stitching other tissue over the repaired ligaments further strengthens the repair.

Lateral ankle ligament seen through an incision |
Tendons may also be used to replace the ligaments. The surgeon weaves a tendon into the bones around the ankle. The tendon is held in place with stitches and possibly a screw in the bone. One option is to use the patient’s own hamstring tendon, which is taken through a separate incision on the inside part of the knee. Another option is to use a cadaver tendon. A different method is to take a portion of one of the tendons from the side of the ankle and weave it into the fibula bone.
What happens after surgery?
You can expect to be in a splint or cast for a minimum of two weeks. It may be up to six weeks before weight can be placed on the ankle. Weight bearing is gradually advanced in a removable walking boot. An athletic ankle brace is typically used after the boot.
Ankle strengthening begins after six weeks as pain and swelling allow. This may involve formal physical therapy. Straight-line running is allowed when the ankle is strong enough for it. Sport-specific exercises can then start gradually. The total expected recovery time is between six and 12 months.
Potential Complications
There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Patients commonly have decreased feeling around their incision. It is also common to have decreased feeling that extends to the top of the foot. This occurs up to 20 percent of the time and ranges from increased sensitivity to complete loss of sensation. Other less common problems include delayed wound healing and infection. Blood clots within the veins of the leg can also occur.
Frequently Asked Questions
What is the risk of retearing my ligament after it has been repaired?
Tearing of the ligament can have many definitions. Complete tearing can occur but usually only after repeat injury. However, repaired ligaments can stretch out over time. Long-term studies that look at these surgeries and patient satisfaction have shown that more than 90 percent of patients have a good or excellent outcome.
What if my ankle instability does not improve after surgery?
The results of surgery vary based on the severity of the initial injury. Outcomes will vary as well. Patients who have persistent instability after surgery may improve with physical therapy or by wearing a brace. Additional surgeries to reconstruct the ligaments may be an option. Ankle fusion could also be considered.
Ankle Fracture Surgery
What is an ankle fracture?
The upper part of the ankle joint comes from the tibia (shin) and the fibula (outer leg). The tibia forms the front, rear and inner part of the ankle joint. The lower fibula forms the outer part of the ankle joint. The ends of these bones are called malleoli. There are two malleoli on the tibia (medial and posterior) and one on the fibula (lateral).
Ankle fractures occur when the malleoli are broken. These fractures are very common. Ankle fractures can happen after falls, car accidents or twisting of the ankle. One, two or all three malleoli can be broken.
Symptoms of an ankle fracture are pain, swelling, bruising and problems with ankle motion. X-rays help show which need treatment from an orthopedic surgeon.
What are the goals of ankle fracture surgery?
The main goal of surgery is to get the ankle joint to heal with a normal shape. Once the ankle is put back together, the next
step is to regain normal movement. The long-term goal of repairing a broken ankle is to decrease the chances of ankle arthritis in the future.
What signs indicate surgery may be needed?
When the ankle fracture is unstable or in bad position, surgery is needed to repair the ankle. In some cases, the bones of the ankle may poke through the skin. These are called open ankle fractures and require surgery.
When should I avoid surgery?
Ankle fracture surgery is not needed if the ankle is in position and stable despite the fracture. Ankle fracture surgery may be too risky when patients have a severe medical condition.
General Details of Procedure
Antibiotics are given shortly before the start of the surgery. Once the patient receives antibiotics and anesthesia, the surgery can safely begin. Incisions are made through the skin of the ankle where the bones are broken. The breaks in the bone are then repositioned and held there with implants. After the ankle fracture is repaired, the patient’s leg is placed in a protective splint made of plaster. Some patients can go home after surgery the same day while others may stay overnight in the hospital.
Specific Technique
Most ankle fracture surgery involves open reduction and internal fixation (ORIF). An incision is made over the ankle to see the fractured bones. Like a jigsaw puzzle, the pieces of the broken bones are placed back together (open reduction). The broken bones are then held together (internal fixation) in this correct position with metal plates and/or screws. This internal fixation provides stability so movement can begin shortly after surgery as the ankle fracture heals.
What happens after surgery?
Surgical treatment of ankle fractures allows patients to regain ankle function while the bones and joint heal. Immediately after surgery, your ankle will be immobilized for a few weeks. Once the wounds are healed, you will be fitted for either a cast or a boot. Many surgeons use a removable boot. The boot protects the ankle as it heals but can be removed to allow washing, wound checks and icing.
Once the broken bones start to heal, you can put weight on the ankle. This starts in the boot. You are then allowed to wean out of the cast or boot. You can return to normal activities once the bones are fully healed. Some patients may need physical therapy for their ankle to regain full movement and strength. While everyone is different, it can take up to a year after surgery for some patients to regain full ankle function.
Potential Complications
There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Problems after ankle fracture surgery include ankle joint stiffness, weakness and arthritis. Possible complications after ankle fracture surgery include infection and problems with healing. The chances of these are higher for patients with certain medical conditions, medicines and lifestyles. Factors that increase risks after ankle fracture surgery include diabetes, steroid use and cigarette smoking.
Frequently Asked Questions
Will my ankle hardware (plate and/or screws) have to be removed at some point?
Plates and screws used to fix an ankle fracture are not removed as long as they are not causing problems. Most people do not have problems with the plate and screws. They are not regularly removed since this would involve another surgery. Rarely, the plate and screws can cause some pain or irritation. When this happens, the hardware may be removed after the fracture is healed.
Will I be awake for my surgery?
There are different types of anesthesia for ankle fracture surgery. Some patients are put asleep. Others can be injected with numbing medicine to make the ankle numb. You may only need to be made sleepy during the surgery so you don’t move.
Ankle Arthroscopy
What is ankle arthroscopy?
Ankle arthroscopy is a minimally invasive surgical procedure that orthopaedic surgeons use to treat problems in the ankle
joint. Ankle arthroscopy uses a thin fiber-optic camera (arthroscope) that can magnify and transmit images of the ankle to a video screen.
What are the goals of ankle arthroscopy?
The goals of surgery are to reduce ankle pain and improve overall function.
What is arthroscopy used for?
Arthroscopy can be used to diagnose and treat different disorders of the ankle joint. The list of problems that can be treated with this technology is constantly evolving and includes:
Ankle arthritis: Ankle fusion is a treatment option appropriate for many patients with end-stage ankle arthritis. Ankle arthroscopy offers a minimally invasive way to perform ankle fusion. Results can be equal to or better than open techniques.
Ankle fractures: Ankle arthroscopy may be used along with open techniques of fracture repair. This can help to ensure normal alignment of bone and cartilage. It may also be used during ankle fracture repair to look for cartilage injuries inside the ankle.
Ankle instability: Ligaments of the ankle can become stretched out, which can lead to a feeling that the ankle gives way. These ligaments can be tightened with surgery. Arthroscopic techniques may be an option for this problem.
Anterior ankle impingement (also referred to as athlete’s ankle or footballer’s ankle): Ankle impingement occurs when bone or soft tissue at the front of the ankle joint becomes inflamed. Symptoms include ankle pain and swelling. This can limit the
ability to bend the ankle up. Walking uphill is often painful. Osteophytes (bone spurs) can be seen on X-ray. Arthroscopy can be used to shave away inflamed tissues and bone spurs.
Arthrofibrosis: Scar tissue can form within the ankle. This can lead to a painful and stiff joint. This is known as arthrofibrosis. Ankle arthroscopy can be used to identify the scar tissue and remove it.
Infection: Infection the joint space cannot be treated with antibiotics alone. It often requires an urgent surgery to wash out the joint. This can be done with arthroscopy.
Loose bodies: Cartilage, bone and scar tissue can become free floating in the joint and form what is referred to as loose bodies. Loose bodies can be painful and can cause problems such as clicking and catching. Locking of the ankle joint may occur. Ankle arthroscopy can be used to find and remove the loose bodies.
Osteochondral defect (OCD): These are areas of damaged cartilage and bone in the ankle joint. OCDs are usually caused by injuries to the ankle such as fractures and sprains. Common symptoms include ankle pain and swelling. Patients may complain of catching or clicking in the ankle. The diagnosis is made with a combination of a physical exam and imaging studies. Imaging may include X-rays, MRI or CT scan. The treatment is based on the size, location and stability of the OCD. The patient’s symptoms and activity demands are also considered. Surgery often consists of scraping away the damaged cartilage and drilling small holes in the bone to promote healing. Bone grafting and cartilage transplant procedures can also be performed.
Posterior ankle impingement: This occurs when the soft tissue at the back of the ankle becomes inflamed. Pointing the foot down can be painful. This overuse syndrome occurs commonly in dancers. It can be associated with an extra bone called an
os trigonum. The problem tissue can be removed with arthroscopy.
Synovitis: The soft tissue lining of the ankle joint (synovial tissue) can become inflamed. This causes pain and swelling. It can be caused by injury and overuse. Inflammatory arthritis (rheumatoid arthritis) and osteoarthritis can also cause synovitis. Ankle arthroscopy can be used to surgically remove inflamed tissue that does not respond to nonsurgical treatment.
Unexplained ankle symptoms: Occasionally patients develop symptoms that cannot be explained by other diagnostic techniques. Arthroscopy provides the opportunity to look directly into the joint. The surgeon can then identify problems that may be treated with surgery.
When should I avoid ankle arthroscopy?
Elective arthroscopy is not appropriate for some patients. Patients with severe ankle arthritis may not benefit from arthroscopic “clean up” surgery. Patients with active infections or other medical problems may also not be appropriate surgical candidates.
General Details of Procedure
The surgeon marks the operative leg prior to surgery. The patient is transported to the operating room and given anesthesia. A tourniquet is commonly applied to the leg. The leg is thoroughly cleaned. The surgeon will sometimes use a device to “stretch” the ankle joint and make it easier to see.
At least two small incisions are made in the front and/or back of the ankle. These “portals” become the entry sites into the ankle for the arthroscopic camera and instruments. Sterile fluid flows into the joint to expand it and allow better visualization. The camera and instruments can be exchanged between portals to perform the surgery. After the surgery is complete, sutures are placed to close the portals. A sterile dressing is placed over the sutures. A splint or boot is often used.
What happens after the procedure?
You can expect some pain and swelling following surgery. The leg may need to be kept elevated. You may need to take oral pain medication for several days. You may be able to walk on the leg immediately, or you may need to wait several months before putting weight on the leg. This will depend on the type of surgery performed and the recommendations of your surgeon. If needed, sutures are removed one to two weeks after surgery. Your surgeon will determine when activities such as range-of-motion and ankle exercises are allowed. Physical therapy may also be used.
Potential Complications
There are complications that can occur with any surgery. These include the risks associated with anesthesia, infection, and bleeding or blood clots.
Potential complications specific to ankle arthroscopy include injury to nerves and blood vessels around the ankle. Numbness or tingling at the top of the foot can occur approximately 10 percent of the time. This typically resolves over time.
Frequently Asked Questions
When can I safely return to driving?
When you are able to bear weight without limitation and are no longer taking narcotic pain medication you will likely be cleared to return to driving.
When can I expect to return to work and sports?
You may be able to return work several days after surgery if you can safely complete your job duties. Most patients can expect to be out of work for at least one to two weeks. It is possible to return to high-level sports following ankle arthroscopy, but expect at least four to six weeks of recovery before getting back to such activities.
What are the outcomes of ankle arthroscopy?
Seventy to 90 percent of patients undergoing ankle arthroscopy for the most common problems achieve good or excellent results.
What are the advantages of ankle arthroscopy?
Ankle arthroscopy allows the surgeon to see inside the ankle with small incisions. This minimizes problems sometimes encountered with large incisions, such as infection and pain. The procedure can be performed as an outpatient because of its minimally invasive nature. Patients may be able to begin rehabilitation sooner, and they may be able to return to high-level activities such as sports more quickly.
Posterior Ankle Endoscopy or Arthroscopy
What is posterior ankle endoscopy/arthroscopy?
Posterior ankle endoscopy/arthroscopy is a technique used to look at and treat problems in the back of the ankle.
| Figure 1: X-ray of the ankle from the side showing the ankle and subtalar joints. |
What is posterior ankle endoscopy/arthroscopy used for?
First, it’s important to understand ankle anatomy. The ankle joint is the joint between the lower leg bones (tibia and fibula) and the ankle bone (talus) (figure 1). The joint below the ankle joint is called the subtalar joint; it lies between the ankle bone and the heel bone (calcaneus). The talus has a bony prominence in the back next to the flexor hallucis longus (FHL) tendon. This is the tendon that moves the big toe downward toward the floor.
The bony posterior prominence might be the cause of ankle pain in some people if it is large (called a trigonal process) or it is not completely fused with the talar bone (called an os trigonum) (figure 2).
Pain might also occur if the FHL tendon gets irritated. This can happen if the tendon doesn’t fit well because the tunnel is too tight or the tendon is too big, or if the tendon is inflamed and swollen (called tenosynovitis).
An ankle sprain may cause a tear of the posterior ankle ligaments. The torn pieces can flip inside the joint. They can get pinched between the joint surfaces and cause pain. This problem is called posterior soft tissue impingement.
The Achilles tendon attaches to the back of the heel bone. It can get pinched by a prominent piece of bone at the top of the heel (called a Haglund’s deformity). This can lead to wear of the Achilles tendon and calcium deposits in the tendon (called insertional Achilles tendonitis).
What signs indicate surgery may be needed?
Patients typically experience pain in the back of of the ankle. The precise location of the pain may differ depending on the cause. The pain from Achilles tendonitis is typically at the surface in back of the heel. This pain often increases when wearing closed shoes and improves with shoes that have open heels (e.g. clogs).
The pain from an os trigonum, an FHL problem or posterior soft tissue impingement tends to be deeper. It typically increases with downward motion of the ankle (pointing the toes). Soccer players and ballet dancers tend to be at higher risk for these problems.
When should I avoid surgery?
You should avoid a posterior ankle endoscopy or arthroscopy if you have Infection in the skin or soft tissue of the posterior ankle area. You should discuss all of your medical conditions with your surgeon before you have this procedure.
General Details of Procedure
With the patient lying face-down or on the side, the orthopaedic foot and ankle surgeon makes incisions at the back of the
| Figure 2: The FHL tendon and part of the FHL muscle seen running beside the os trigonum. |
ankle. Typically two incisions are made on either side of the Achilles tendon. An arthroscope (a tube-shaped device with a camera at the tip) is inserted and allows the surgeon to see the area. Fatty tissue at the back of the ankle is removed to create a workspace. The FHL tendon is identified and the blood vessels and nerves are protected. A small part of the posterior ankle capsule might need to be removed in order to enter the ankle joint. A device that “stretches” the ankle joint is often used to help with visualization.
The problem causing the pain is identified and treated accordingly using various small instruments:
- The os trigonum is freed from the surrounding soft tissues then removed.
- The FHL tenosynovitis is cleaned up using a shaver and the tunnel is released if necessary.
- The torn ligaments causing posterior soft tissue impingement are cleaned up with the shaver.
- The Haglund’s deformity is removed using a burr.
What happens after surgery?
The post-operative dressing is usually a splint or bulky soft dressing. A post-op shoe or boot may be added for protection. Weight bearing may be restricted depending on the surgery that is done. Always ask your surgeon about postoperative weight bearing.
Foot elevation is encouraged in the first 48 hours after the procedure. The stitches are removed in 10 to 14 days and more aggressive exercises can be started thereafter. Early motion of the ankle and foot joints is typically recommended. Formal physical therapy may be ordered. A night splint to keep the ankle at 90 degrees may be used to prevent tightening of the posterior ankle soft tissue.
Potential Complications
Injury to blood vessels and nerves is uncommon but remains a complication of this procedure. Other complications include numbness on the bottom of the foot, very sensitive skin on the outside part of the foot, Achilles tendon tightness, chronic pain syndrome, infection, and the formation of a cyst at the incision site.